Ensuring Success of PM’s Plan

Association of Healthcare Providers (India) presents 5-priority areas that require utmost attention to support the Modi government’s 100-day plan, which will specify the roadmap to take India to healthier heights….
By Dr Girdhar Gyani
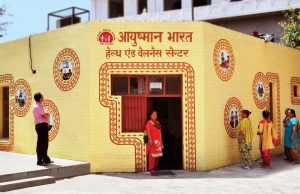
Healthcare, of late, has come into greater focus by the government that had right in the beginning of its earlier term too had announced National Health Assurance Mission, which is synonymous with universal health coverage. This was followed up with National Health Policy in the year 2017 and year later the government launched the world’s largest healthcare scheme under the name AYUSHMAN BHARAT (AB). The two components of the AB scheme i.e. 1.5 lakh Health & Wellness Centres and Prime Minister Jan Arogya Yojana (PMJAY), providing insurance cover up to Rs 5-lakh per family under designated underprivileged sections of society are by all standards very ambitious/path-breaking and once get implemented will usher, a New India: Healthy India.
Prime Minister Narendra Modi in his first interaction with new ministers has directed them to come out with a 100-day plan, which will specify roadmap for coming years to take India to newer heights. Association of Healthcare Providers (India) is fully committed to support government’s healthcare initiatives in line with its motto; ‘Educating & Advocating for Well Being of Common Man’. The 100-day blue-print as we understand, will develop framework for coming years. In our considered opinion, we have outlined 5-priority areas, which could be part of framework to make AYUSHMAN BHARAT as India’s great success story, which has potential to be the role model scheme for other developing nations.

INFRASTRUCTURE: For achieving ‘Health for All’ the first and foremost step has to be to ensure that we have necessary infrastructure in terms of healthcare establishments. India has currently about 1-bed per 1000-population, against the suggested WHO norm of 3.5- beds per 1000 for developing nations. We need to augment it on a war footing in public and private sector. Prime Minister Narendra Modi has suggested to have 3000 new hospitals to cope up with the shortage of beds. There is gross geographical inequality as most tertiary care beds are confined within TIER-I/II cities, making healthcare inaccessible to large majority of population.
As an example, Telangana has 167-hospitals with bed size of 100-and above, out of which 150-hospitals are in Hyderabad. Same is the story in all other states. The private sector is credited with about 85% of tertiary care beds and these are primarily in tier-I and some in tier-II cities. The Union government needs to proactively engage with private sector to open 100-bedded hospitals in Tier-III cities. There are some genuine issues about sustainability and if these are addressed, we can have these number of secondary/tertiary care hospitals in deficient areas in next 3-years.
 MANPOWER: India has currently half of recommended figure of 23-healthcare workforce per 10,000 populations. We have about 1-doctor per 1600 population against WHO norm of 1-doctor per 1000. We have huge shortage of specialists. To cite the government figure, there is 80% shortage of specialists in 5500 Community Health Centres (CHCs). The Government need to come out with innovative models to make up this shortage i.e. increase of PG seats in medical colleges, increase of DNB seats, recognizing of diploma program run by College of Physicians & Surgeons in various specialties. The government may consider recognizing Fellowships by various specialty associations.
MANPOWER: India has currently half of recommended figure of 23-healthcare workforce per 10,000 populations. We have about 1-doctor per 1600 population against WHO norm of 1-doctor per 1000. We have huge shortage of specialists. To cite the government figure, there is 80% shortage of specialists in 5500 Community Health Centres (CHCs). The Government need to come out with innovative models to make up this shortage i.e. increase of PG seats in medical colleges, increase of DNB seats, recognizing of diploma program run by College of Physicians & Surgeons in various specialties. The government may consider recognizing Fellowships by various specialty associations.
There is great imbalance in geographical distribution of medical colleges, which need to be urgently arrested. The plan for allowing some of selected 300+ bed private hospitals in deficient districts to have attached academic blocks for 100-MBBS seats can be quickly put in place. The government can open 10-institues like PGI Chandigarh to operate only PG courses. It needs to be stressed that any amount of increase in healthcare expenditure will not achieve desired outcomes, unless we address the manpower issue.
 Nursing profession is in a dire state. Parents today do not encourage their children to go for nursing career. The nurses have hardly any career progression. The salary for GNM/B.Sc. nurse in many states is below 10,000/, while the salary of driver in these states is above 15000/. The nurses have huge potential to support doctor in clinical work, but they cannot even prescribe a basic pain killer. Indian Nursing Council need to be revamped on priority the way it is being done with MCI. Same is the case with Allied & Healthcare Workforce Council, which has huge potential in providing employment to young population.
Nursing profession is in a dire state. Parents today do not encourage their children to go for nursing career. The nurses have hardly any career progression. The salary for GNM/B.Sc. nurse in many states is below 10,000/, while the salary of driver in these states is above 15000/. The nurses have huge potential to support doctor in clinical work, but they cannot even prescribe a basic pain killer. Indian Nursing Council need to be revamped on priority the way it is being done with MCI. Same is the case with Allied & Healthcare Workforce Council, which has huge potential in providing employment to young population.
RESTRUCTURING OF GOVERNMENT HEALTH INSURANCE SCHEMES: The Government has launched ambitious scheme by way of PMJAY/AYUSHMAN BHARAT. It is a bold step towards making the country achieve universal health coverage. The scheme is presently designed to cover 40% of India’s population. If we add some of the additional population, presently under medical cover like state schemes, CGHS/ECHS/ESIC and private insurance, we may be approaching 70% of population getting health insurance. This is going to be huge number and milestone to put India achieving universal health coverage. As mentioned earlier, about 85% tertiary care beds are with private sector and therefore operation of such government insurance schemes will need to involve the private sector.
There is considerable discrepancy in fixing of rates of medical procedures under these schemes. The government needs to undertake costing exercise of medical procedures in various settings like category of city and level of specialization. Considering that no new investment is coming in hospital industry, big hospital chains are either undergoing merger or being taken over by foreign investors and even many of hospitals are closing down, it is necessary that we address financial sustainability issue confronting the hospital industry on a priority basis.
PATIENT SAFETY: The Harvard Institute of Public Health came out with the finding that India was reporting 5.2 million medical errors annually. Same is the case with many developing and even developed nations. There are medical errors arising out of hospital acquired infection and in prescription/dispensing of medication. For want of any designed framework, these go un-noticed. We are stressing on making healthcare affordable but not talking about following the clinical protocols, and monitoring of medical errors under the overall framework of patient safety.

There is established fact that hospitals, if pushed to lower limits of sustainability, will compromise on patient safety, which in time to come may prove costly in terms of increase in disease burden. NABH Accreditation, launched in the year 2006 has succeeded in bringing focus on patient safety. However as on date only 2-3% of hospitals/nursing homes have implemented NABH standards. We have a long way to go in practicing of patient safety. We have to make regulation simple, focused around patient safety and enforce it effectively. The Ministry of Health and Family Welfare (MoHFW) has recently come out with Patient Safety Implementation Framework (2018-25), which should be promoted through government, associations and NGOs. These measures have big role in containing morbidity/mortality, which presently we do not even monitor or measure.
PROMOTIVE/PREVENTIVE HEALTHCARE: Health & Wellness Centres under AYUSHMAN BHARAT, once implemented will bring major change. This will bring back emphasis on primary care and referral mechanism, which has been missing. Even today, majority of patients travel long distances to arrive at AIIMS for primary care. We need to strengthen CHCs and District Hospitals.
The use of technology by way of telemedicine and home health will have to be adopted in big way, more so when we have huge shortage of manpower. MoHFW came out with standards for electronic health records (EHR) which have huge potential in transferability of health data without which patient are made to undergo repeated diagnostic tests etc. But we have not made any headway in that direction.
While all these years focus has been on providing curative part of healthcare, we have missed out the gold mine by way of not focusing on promotive and preventive healthcare. Health & Wellness Centres hopefully will bridge this gap. This, in fact, can save huge expenditure on curative healthcare with bonus coming by reducing suffering to the mankind.
There are major issues related to sanitation, drinking water and nutrition, which have huge bearing on preventive healthcare. These aspects are being pursued by different ministries. The challenge is to integrate their initiatives to achieve common objectives. We need to educate communities through governments (Municipalities, Gram Panchayats) and NGOs on preventive health aspects. We have successfully implemented INDRADHANUSH for children, we need to likewise promote‘Adult Vaccination’, which has huge potential in preventing many diseases.
(The author is Secretary General, Association of Healthcare Providers, India)