Sugar Steals Sight
Diabetic retinopathy is one of the most devastating — yet preventable — complications of diabetes. High blood sugar silently damages the tiny vessels in the retina, leading to leakage, swelling, and, in severe cases, blindness.
By Dr Shishir Narayan

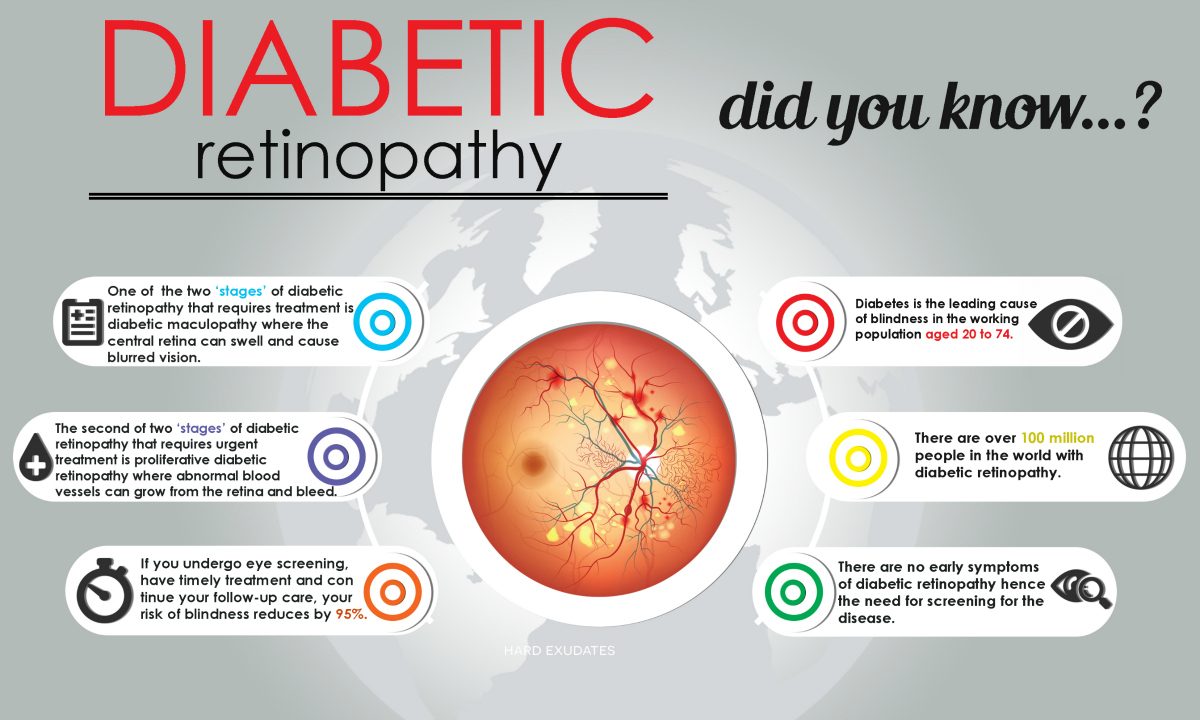
If you are diabetic, finding and treating eye disease early — before it causes vision loss or blindness — is one of the best investments you can make in your health. With the number of diabetics in India now exceeding 101 million, diabetic retinopathy has emerged as a leading cause of avoidable blindness. The World Health Organization (WHO, 2024) estimates that one in three diabetics will eventually develop some form of retinopathy, making regular screening indispensable.
If you experience floating spots or dark strings, blurred or fluctuating vision, impaired colour perception, or dark or empty areas in your visual field, you may be suffering from diabetic retinopathy. In simple terms, this is a complication of diabetes that affects the eyes. Left untreated, it can progress silently and result in irreversible blindness.
Diabetic retinopathy remains the most common cause of vision loss among people with diabetes and is a major cause of blindness among working-age adults. The disease results from damage to the tiny blood vessels of the retina — the light-sensitive layer at the back of the eye that acts like the film in a camera. Persistent high blood glucose weakens the retinal capillaries, causing leakage, blockage, and abnormal new vessel growth, ultimately compromising sight.
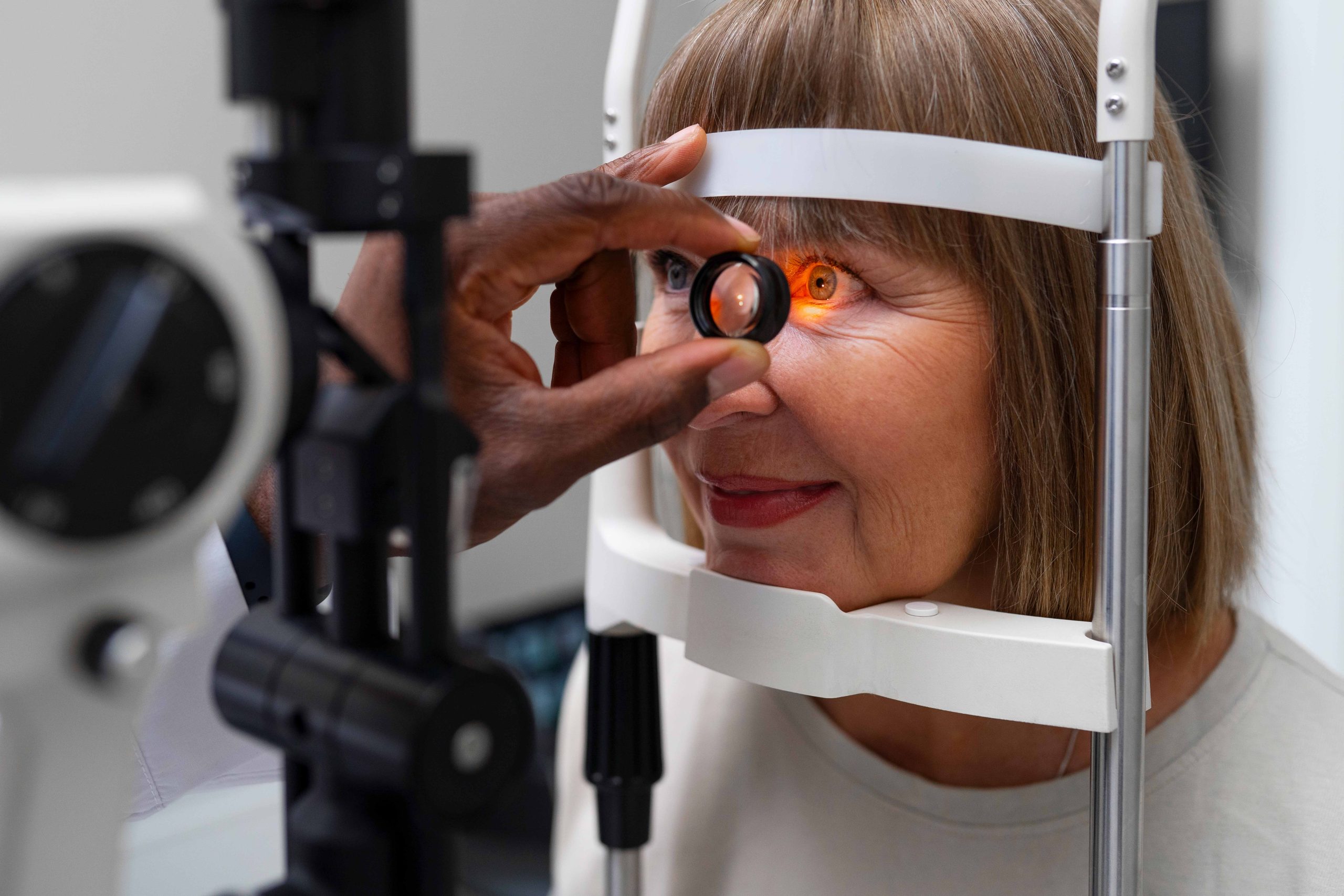
Early detection makes a world of difference. Effective treatments such as laser therapy, anti-VEGF injections, and vitrectomy are available, but they work best before any significant vision loss has occurred. This is why comprehensive, dilated eye examinations are recommended for every diabetic at least once a year.
 How Diabetes Affects the Eye
How Diabetes Affects the Eye
Elevated blood glucose can damage the body in multiple ways, but its effect on the eye’s delicate blood vessels is particularly devastating. High sugar levels trigger inflammation and oxidative stress, thickening vessel walls and causing tiny leaks of blood or fluid. Over time, poor circulation in the retina leads to oxygen deprivation. The eye, in a desperate attempt to compensate, produces fragile new blood vessels — a process known as neovascularisation. These new vessels are weak and prone to bleeding, setting off a cascade that can result in permanent vision impairment.
The longer diabetes remains uncontrolled, the greater the cumulative injury to the retina. Hypertension, kidney disease, and high cholesterol accelerate this damage, which is why integrated management of all metabolic risk factors is vital.
 Symptoms of Retinopathy
Symptoms of Retinopathy
In its early stages, diabetic retinopathy often causes no symptoms at all. This deceptive silence is what makes the disease so dangerous. As it progresses, patients may notice blurred or fluctuating vision, dark spots, colour distortion, or difficulty focusing. Typically, both eyes are affected.
With proper medical management and timely eye care, vision loss can be prevented or slowed. Pregnancy can temporarily worsen diabetic retinopathy, so expectant mothers with diabetes require additional eye examinations throughout gestation. Any sudden change in vision — blurriness, haziness, or dark patches — should prompt immediate consultation with an ophthalmologist.
Over time, excessive blood sugar can block the small vessels that nourish the retina, forcing the eye to grow new, abnormal ones. Unfortunately, these vessels are structurally defective — they leak easily and may pull on the retina, causing detachment or haemorrhage.
Types and Progression of Diabetic Retinopathy
There are two major stages of diabetic retinopathy:
Early Diabetic Retinopathy (Non-Proliferative Diabetic Retinopathy – NPDR)
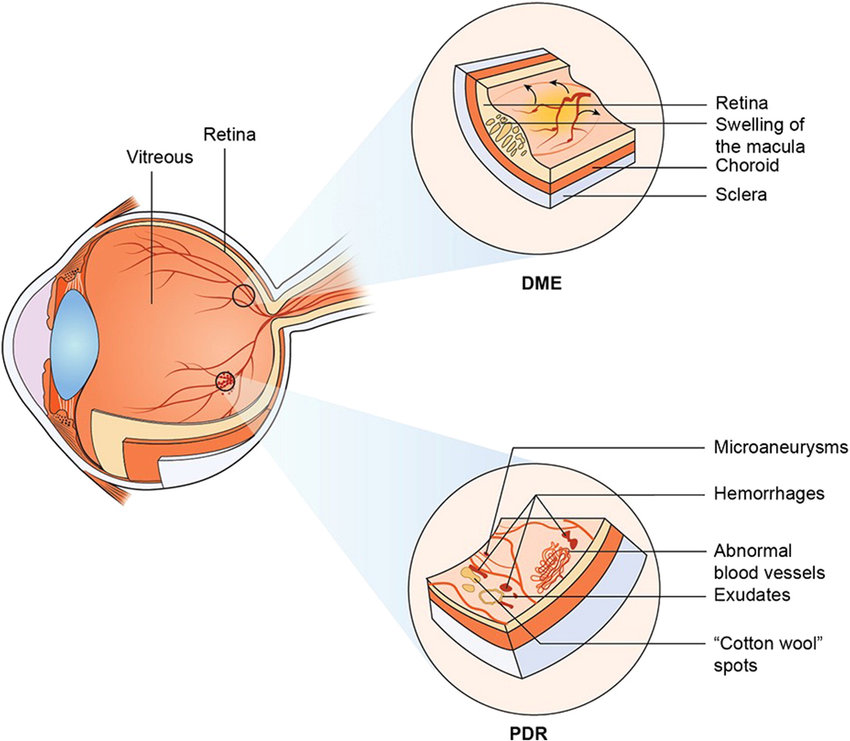
This is the initial and more common form of the disease. In NPDR, the walls of retinal blood vessels weaken, forming tiny bulges called micro-aneurysms that may leak blood or fluid into the retina. Larger vessels can become irregular and dilated, leading to patchy areas of poor circulation. As NPDR progresses from mild to severe, the risk of macular oedema — swelling of the central retina responsible for sharp vision — increases significantly.
After about twenty years of diabetes, most patients show some signs of NPDR. Although this stage is not always sight-threatening, untreated macular oedema can cause serious central vision loss.
 Proliferative Diabetic Retinopathy (PDR)
Proliferative Diabetic Retinopathy (PDR)
This advanced stage poses a far greater risk. When retinal blood vessels close off, the retina compensates by growing new, abnormal vessels. These may extend into the vitreous — the clear, gel-like centre of the eye — and are prone to bleeding. PDR can cause vitreous haemorrhage, retinal detachment, or secondary glaucoma, all of which can result in severe vision loss or blindness. Scar tissue from neovascularisation may also contract, pulling the retina away from its base, a condition requiring urgent surgery.
In both NPDR and PDR, macular oedema is the most common cause of visual impairment, affecting nearly 7 percent of diabetics globally (International Agency for the Prevention of Blindness, 2024).
Complications of Advanced Retinopathy
In advanced stages, diabetic retinopathy can produce several complications:
Vitreous haemorrhage occurs when new blood vessels bleed into the vitreous cavity. Minor bleeding may cause small floaters or dark spots; severe bleeding can obscure vision entirely. Fortunately, the blood often clears naturally within weeks or months, and vision usually recovers if the retina remains intact.
Retinal detachment results when scar tissue pulls the retina away from the back of the eye. This can cause flashes of light, floating shapes, or a sudden curtain-like shadow across vision. Immediate surgical intervention is required.
Neovascular glaucoma develops when new vessels grow over the drainage angle at the front of the eye, blocking fluid outflow and raising intraocular pressure. The optic nerve becomes damaged, leading to irreversible blindness if untreated. Diabetics with long-standing disease are therefore urged to have their eye pressure measured regularly during check-ups.
Treatment and Prevention
Laser photocoagulation remains a cornerstone of treatment for diabetic retinopathy. The procedure seals leaking blood vessels and prevents further abnormal growth. When performed in time, laser therapy and follow-up care can reduce the risk of blindness by up to 90 percent (American Academy of Ophthalmology, 2023). The treatment is usually performed in an ophthalmologist’s clinic under local anaesthesia. Though generally painless, patients may experience mild discomfort or difficulty adjusting to darkness for a few days.
For cases involving macular oedema or proliferative changes, anti-VEGF (vascular endothelial growth factor) injections such as ranibizumab or aflibercept have revolutionised outcomes, restoring measurable vision in many patients. In more advanced cases where vitreous bleeding or scar tissue threatens retinal detachment, vitrectomy — a microsurgical procedure that removes the cloudy gel from inside the eye — can successfully restore sight in over 70 percent of cases (Lancet Ophthalmology 2024).
Beyond medical intervention, prevention is paramount. Maintaining optimal blood-sugar levels, controlling blood pressure and cholesterol, and avoiding smoking are essential. Recent clinical evidence shows that every 1 percent reduction in HbA1c lowers the risk of retinopathy progression by 35 percent. A comprehensive eye examination with dilation should be performed at least once a year — more frequently for those with long-standing or poorly controlled diabetes.
Living with Diabetes and Protecting Vision
Finding and treating diabetic retinopathy early — before vision is affected — remains the best way to preserve sight. With modern technology, including optical coherence tomography (OCT) and fundus photography, even subtle retinal changes can now be detected years before symptoms arise.
If you have diabetes, commit to yearly eye exams, maintain a healthy diet, engage in regular exercise, and keep your blood pressure under control. Integrating ophthalmic care into routine diabetes management — a practice now endorsed by the All India Ophthalmological Society — can dramatically reduce avoidable blindness in the country.
In short, the eyes are not only the windows to the soul but also the mirrors of metabolic health. By keeping your glucose, blood pressure, and lifestyle in balance, you can protect not just your vision, but your overall quality of life.
(The author is Senior Eye Consultant, Eye Trust, and associated with Shroff Eye Hospital, New Delhi.)

