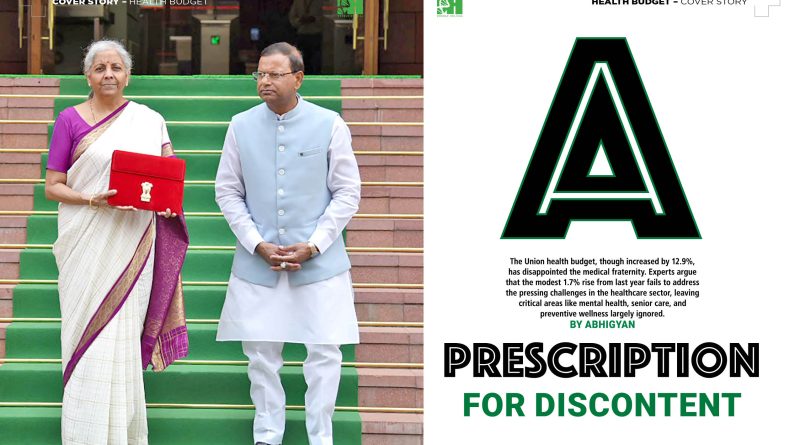
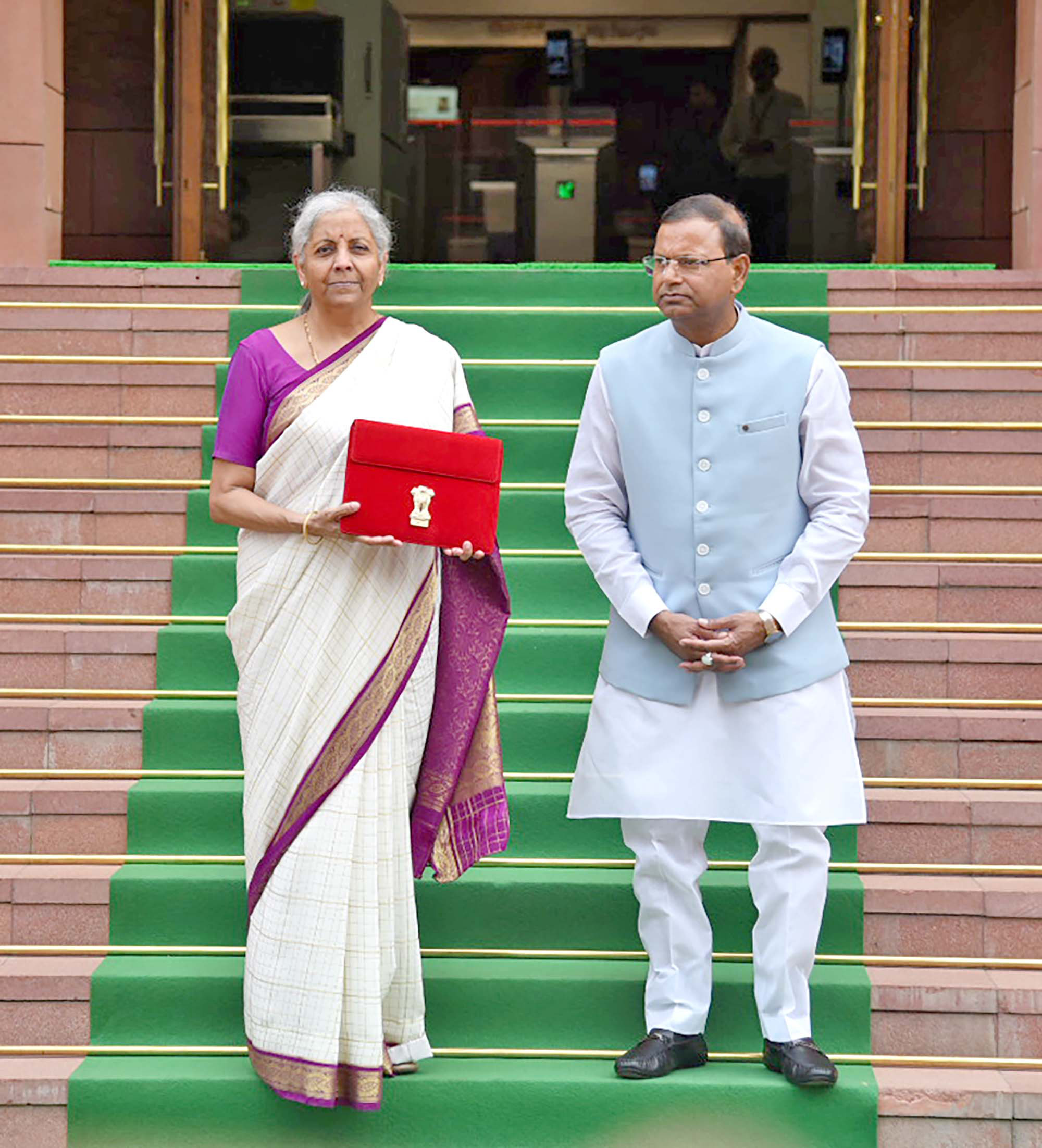
A Prescription for Discontent
The Union health budget, though increased by 12.9%, has disappointed the medical fraternity. Experts argue that the modest 1.7% rise from last year fails to address the pressing challenges in the healthcare sector, leaving critical areas like mental health, senior care, and preventive wellness largely ignored.
By Abhigyan

The Union government for 2024-2025 has allocated ₹90,958.63 crore to the Ministry of Health and Family Welfare, marking a 12.9% increase from the previous year’s revised estimate of ₹80,517.62 crore. Despite this increase, the allocation has left the medical fraternity disillusioned. Experts have pointed out that this budgetary enhancement, when closely examined, translates to a mere 1.7% rise in the overall health budget from the previous financial year, 2024. Furthermore, the budget lacks any substantial new initiatives or announcements that would address the pressing challenges facing the healthcare sector.
One of the few specific measures introduced in the budget is the exemption of customs duty on three cancer treatment drugs: Trastuzumab Deruxtecan, Osimertinib, and Durvalumab. This step, while welcome, appears inadequate in the face of the growing cancer crisis in India. In 2022 alone, India reported over 14.13 lakh new cancer cases and saw a staggering 9.16 lakh deaths attributed to the disease. The exemption, though beneficial, does not address the broader need for a comprehensive cancer care strategy that could encompass prevention, early detection, and treatment across the country.
The budget also introduced reductions in customs duty rates on X-ray tubes and flat panel detectors, which, while useful for medical imaging, again seem like a piecemeal approach in the absence of a holistic plan to strengthen healthcare infrastructure.
The Economic Survey 2024, tabled in Parliament on July 22, highlighted two critical health concerns: the alarming rise in obesity and the burgeoning mental health crisis. The survey drew a direct correlation between the increasing prevalence of obesity in India and the consumption of processed foods, sugars, and unhealthy fats. It underscored the necessity for a national shift towards a healthier lifestyle, emphasising that such a transition is vital for India to fully capitalise on its demographic dividend.
The survey also noted that the surge in the consumption of highly processed, sugar-laden foods, combined with declining physical activity and limited access to diverse and nutritious foods, has exacerbated both micronutrient deficiencies and obesity rates. Alarmingly, the percentage of men aged 18-69 who are classified as obese has increased from 18.9% in NFHS-4 (National Family Health Survey) to 22.9% in NFHS-5. For women in the same age bracket, the figures have risen from 20.6% to 24%, signalling a significant public health challenge.

Mental health, another area of concern, was also given considerable attention in the Economic Survey, which described it as being “intertwined with all aspects of health, namely physical, social, and emotional.” Despite this recognition, the budget’s response appears limited. The allocation for the National Tele Mental Health Programme was increased from ₹65 crore to ₹90 crore—a positive step, but one that falls short of the scale required to address the widespread mental health issues in the country. The National Mental Health Survey 2015-16 revealed that 10.6% of Indian adults suffer from mental health disorders, with treatment gaps ranging between 70% and 92% across different conditions. This stark reality necessitates a far more robust financial and policy commitment than what the current budget offers.
 Dr A K Aggarwal, Medical Advisor for Innovation and Clinical Research at Apollo Group of Hospitals, New Delhi, expressed concern over the rising impact of internet usage on mental health. He cited a 2021 study by the National Commission for Protection of Child Rights, which found that 23.8% of children use smartphones while in bed, and 37.2% experience reduced levels of concentration due to smartphone use. This highlights the growing need for targeted mental health interventions, particularly for the younger population.
Dr A K Aggarwal, Medical Advisor for Innovation and Clinical Research at Apollo Group of Hospitals, New Delhi, expressed concern over the rising impact of internet usage on mental health. He cited a 2021 study by the National Commission for Protection of Child Rights, which found that 23.8% of children use smartphones while in bed, and 37.2% experience reduced levels of concentration due to smartphone use. This highlights the growing need for targeted mental health interventions, particularly for the younger population.
 Reflecting on the budget, Dr Alexander Thomas, President of the Association of Healthcare Providers India (AHPI), described it as a disappointing outcome for the healthcare sector. “Many of our expectations were not met, despite AHPI being specifically invited to the pre-budget meeting,” he said. “We had hoped for a positive shift, particularly in the area of prevention and wellness, which has been almost entirely overlooked—an oversight that is deeply discouraging.”
Reflecting on the budget, Dr Alexander Thomas, President of the Association of Healthcare Providers India (AHPI), described it as a disappointing outcome for the healthcare sector. “Many of our expectations were not met, despite AHPI being specifically invited to the pre-budget meeting,” he said. “We had hoped for a positive shift, particularly in the area of prevention and wellness, which has been almost entirely overlooked—an oversight that is deeply discouraging.”
Dr Thomas further noted the absence of provisions for senior citizens, expressing concern over their exclusion from the budget. “Though we remain hopeful that our advocacy will prompt reconsideration, especially regarding GST aspects, overall, this budget fails to adequately address the critical needs of the health sector. It is vital for policymakers to understand that good healthcare leads to a productive and progressive nation. We must continue to advocate for the healthcare priorities that will uplift our society as a whole.”
 Dr Vinay Aggarwal, Past National President of the Indian Medical Association (IMA), echoed these sentiments, stating, “We have long demanded an increased allocation of financial resources in the Union health budget, advocating for a tax-based system of health financing. In a letter addressed to Finance Minister Nirmala Sitharaman, the IMA expressed concern over the government’s low spending on health. Under various administrations, health allocation has ranged from 1.1% to 1.6% of GDP, placing India among the lowest in the world. This budget does little to change that.”
Dr Vinay Aggarwal, Past National President of the Indian Medical Association (IMA), echoed these sentiments, stating, “We have long demanded an increased allocation of financial resources in the Union health budget, advocating for a tax-based system of health financing. In a letter addressed to Finance Minister Nirmala Sitharaman, the IMA expressed concern over the government’s low spending on health. Under various administrations, health allocation has ranged from 1.1% to 1.6% of GDP, placing India among the lowest in the world. This budget does little to change that.”
Thus, the modest rise in allocation for healthcare does little to meet the escalating demands posed by an aging population, a growing mental health crisis, and the rising burden of non-communicable diseases like cancer and obesity. The lack of substantial provisions for preventive healthcare, senior citizen care, and a more comprehensive mental health framework reflects a budget that is reactive rather than proactive. To build a truly resilient healthcare system, policymakers must go beyond incremental changes and embrace a bold vision that prioritises health as the foundation of national progress.