Childhood Epilepsy The most common neurological disorders….

Epilepsy is one of the most common childhood neurological disorders. It is characterised by recurrent episodes of seizures, which may have a long-term impact on the child’s overall health and development…
By Dr Sheffali Gulati / Dr Gautam Kamila
The incidence of epilepsy differs between developed and developing countries. In Western countries, new cases per year are estimated to be 33.3–82/100,000, in contrast to the maximum incidence of 187/100,000 estimated in developing countries.
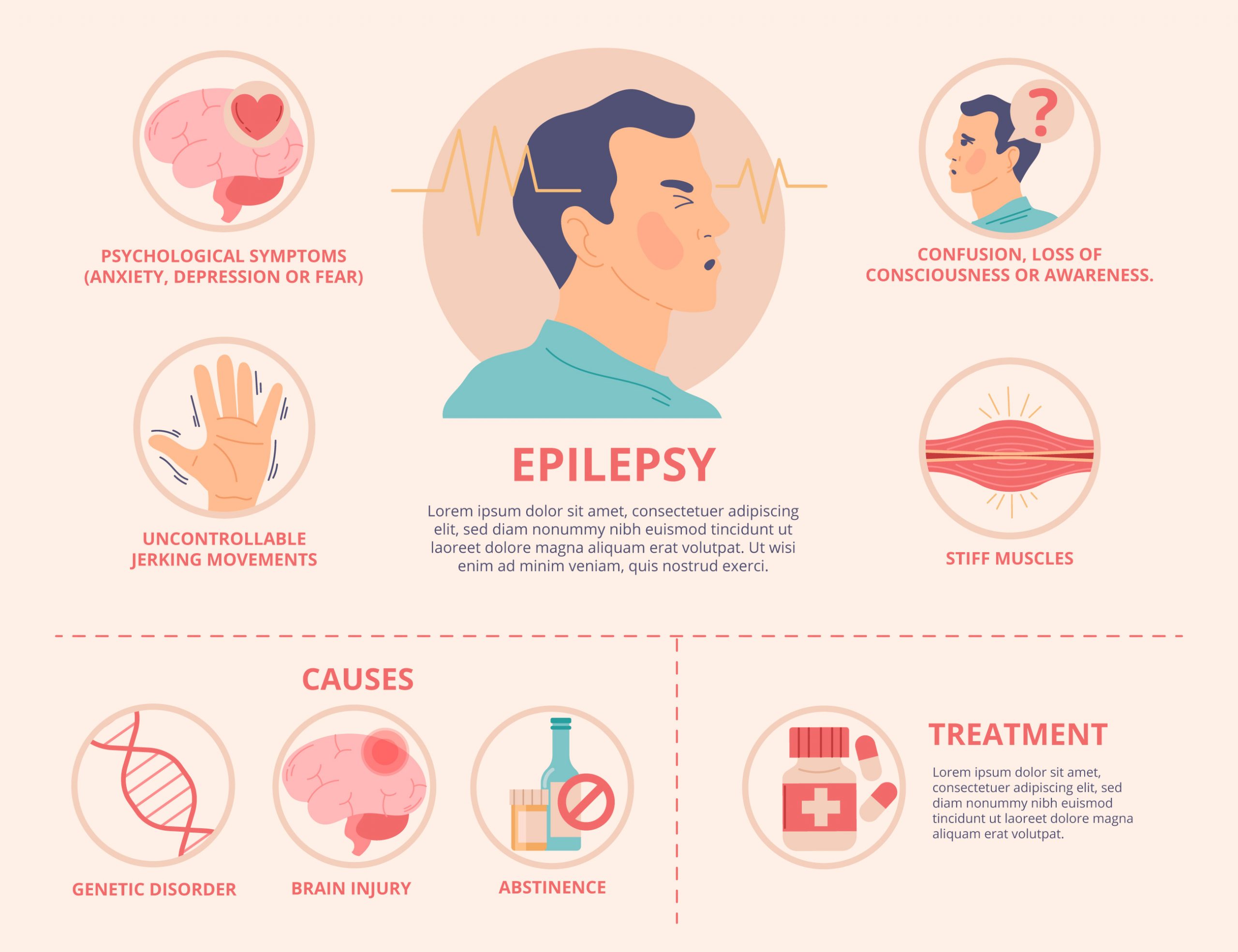
In common parlance epilepsy is a disorder in which nerve cell activity in the brain is disturbed, causing seizures. Epilepsy may occur as a result of a genetic disorder or an acquired brain injury, such as a trauma or stroke.
Abnormal brain development or brain injuries, infection, inflammation, or specific gene mutations can all lead to seizures. The common symptoms of epilepsy includes Staring, Jerking movements of the arms and legs, Stiffening of the body, Loss of consciousness, breathing problems or stopping breathing, loss of bowel or bladder control and falling suddenly for no apparent reason, especially when associated with loss of consciousness.
Recent studies have shown that the maximum incidence occurs in the first year of age with a rate of 102/100,000 cases per year, just like the age range from 1 to 12 in children from 11 to 17 years old incidence is 21–24/100,000 cases. Previous studies suggest that the total incidence of epilepsy is constant from 25 years, showing a slight increase in males .In Italy, epilepsy incidence is 48.35/100,000 new cases per year and it is comparable with data recorded in the other industrialized countries. The peak of incidence occurs in children younger than 15 years old (50.14/100,000 new cases per year) and especially in the first year of life with an incidence of 92.8/100,000 new cases per year. The brain in children is more susceptible to seizures as well as refractory to the consequences of an acute attack.

What are seizures?
Seizures are defined as a transient occurrence of signs and symptoms due to the abnormal, excessive, or synchronous neuronal activity in the brain characterized by abrupt and involuntary skeletal muscles activity. There is a clear onset and remission in a seizure. Status epilepticus (SE) results either from the failure of the mechanisms responsible for termination of seizure or from the initiation of a mechanism, which leads to abnormally, prolonged seizures (for a time period of 5 min or more). It is a condition, which can have long-term consequences (especially if its duration is more than 30 min) including neuronal death, neuronal injury, and alteration of neuronal network, depending on the type and duration of seizures. Febrile seizures are defined as seizures which occur in children aged between 1 month and 6 years with temperature rise over 38 ˚C and without signs of infectious disease of the central nervous system (CNS).
In 2014 the International League Against Epilepsy (ILAE) Task Force proposed the operational (practical) clinical definition of epilepsy, intended as a disease of the brain defined by any of the following conditions:
- At least two unprovoked (or reflex) seizures occurring greater than 24 h apart.
- One unprovoked (or reflex) seizure and a probability of further seizures similar to the general recurrence risk (at least 60%) after two unprovoked seizures, occurring over the next 10 years.
- From 2015 to 2017, the concepts, definition, and classification of seizures, epilepsy, and status epilepticus, were revised by the ILAE Task Force.
How do we investigate a child presenting with seizure?
When a child presents with seizures, a diagnosis is made by the physician, after working through several critical steps, excluding, however, any possibility of seizure mimics. Wherever possible, an etiology of the individual’s epilepsy should be sought for. The most common causes of status epilepticus in children are fever and infections of the CNS. Other causes include hyponatremia, accidental ingestion of toxic agents, abnormalities of the CNS, genetic and metabolic disorders (phenylketonuria, hypocalcemia, hypoglycemia, hypomagnesemia).
 The pathophysiological course of status epilepticus in children depends on the absence of anatomical abnormalities and pre-existing predisposing conditions of CNS.There is a strong correlation between seizures in children and positive family history, high temperature, mental disability, delayed discharge from NICU or premature birth, etc.
The pathophysiological course of status epilepticus in children depends on the absence of anatomical abnormalities and pre-existing predisposing conditions of CNS.There is a strong correlation between seizures in children and positive family history, high temperature, mental disability, delayed discharge from NICU or premature birth, etc.
What is the risk of recurrence of seizures in children?
There is an increased probability of recurrence of seizures in 30% of children with first episode of seizures. The risks factors of recurrent febrile seizures include: small age, duration of first episode of seizures, low temperature during the first episode, positive family history for febrile seizures in a first degree relative, short timeframe from temperature elevation and seizure onset. Children with any of the above risk factors show greater than 70% probability of recurrence of seizure; in contrast patients with none of them have less than 20% probability of recurrence of seizure.
How does seizure happen?
The exact mechanism of seizure onset is not clearly elucidated yet. There are two possible mechanisms which include – either a deficit of neuronal inhibition or an excess of excitatory stimuli. It has been hypothesised that the onset of seizures depends on a deficit in the neuronal inhibition, in particular ý-Aminobutyric acid (GABA) deficit, the most important neurotransmitter of CNS; alternatively it depends on the alteration of the GABA function which determines prolonged and high intensity stimulation. Glutamate receptors, the most important excitatory receptor of CNS, are also involved in seizure physiopathology.
 Preliminary studies in children have confirmed the hypothesis that inflammatory mediators like IL-1 could cause an increase in neuronal stimulation and the onset of febrile seizures,but its clinical and pathological meaning is still unclear. Viral infections are considered to be involved in the pathogenesis of seizures and studies have shown that HHV-6 (Human herpes virus-6) and Rubivirus could be found in 20% of patients affected by febrile seizures for the first time.
Preliminary studies in children have confirmed the hypothesis that inflammatory mediators like IL-1 could cause an increase in neuronal stimulation and the onset of febrile seizures,but its clinical and pathological meaning is still unclear. Viral infections are considered to be involved in the pathogenesis of seizures and studies have shown that HHV-6 (Human herpes virus-6) and Rubivirus could be found in 20% of patients affected by febrile seizures for the first time.
How to manage a seizure in a child?
American Association of Pediatrics (AAP) guidelines on management of febrile seizures suggest not performing diagnostic tests routinely, including lumbar puncture, except if it is necessary based on the state of the condition. A lumbar puncture is firmly recommended in all patients under one-year age that present temperature and seizures. Neuroimaging is advised during the first clinical presentation of seizures and in clinical conditions that could increase the risk of complications. Computerised Tomography (CT) of brain without contrast media is the first test recommended to diagnose traumatic injury to head, hemorrhagic stroke, neurocysticercosis, etc., while a contrast enhanced CT Brain is done to confirm suspected diagnosis of brain tumors or CNS infections. EEG should be considered in all cases of status epilepticus. Etiological evaluation for the cause of seizure should run in parallel with the management of seizures.
Goals of management in status epilepticus
The main goal in management during Status Epilepticus is to stop seizures before neural cells are irreversibly damaged. Thus, early and prompt management of seizures is important to prevent irreversible damage to the neurons.
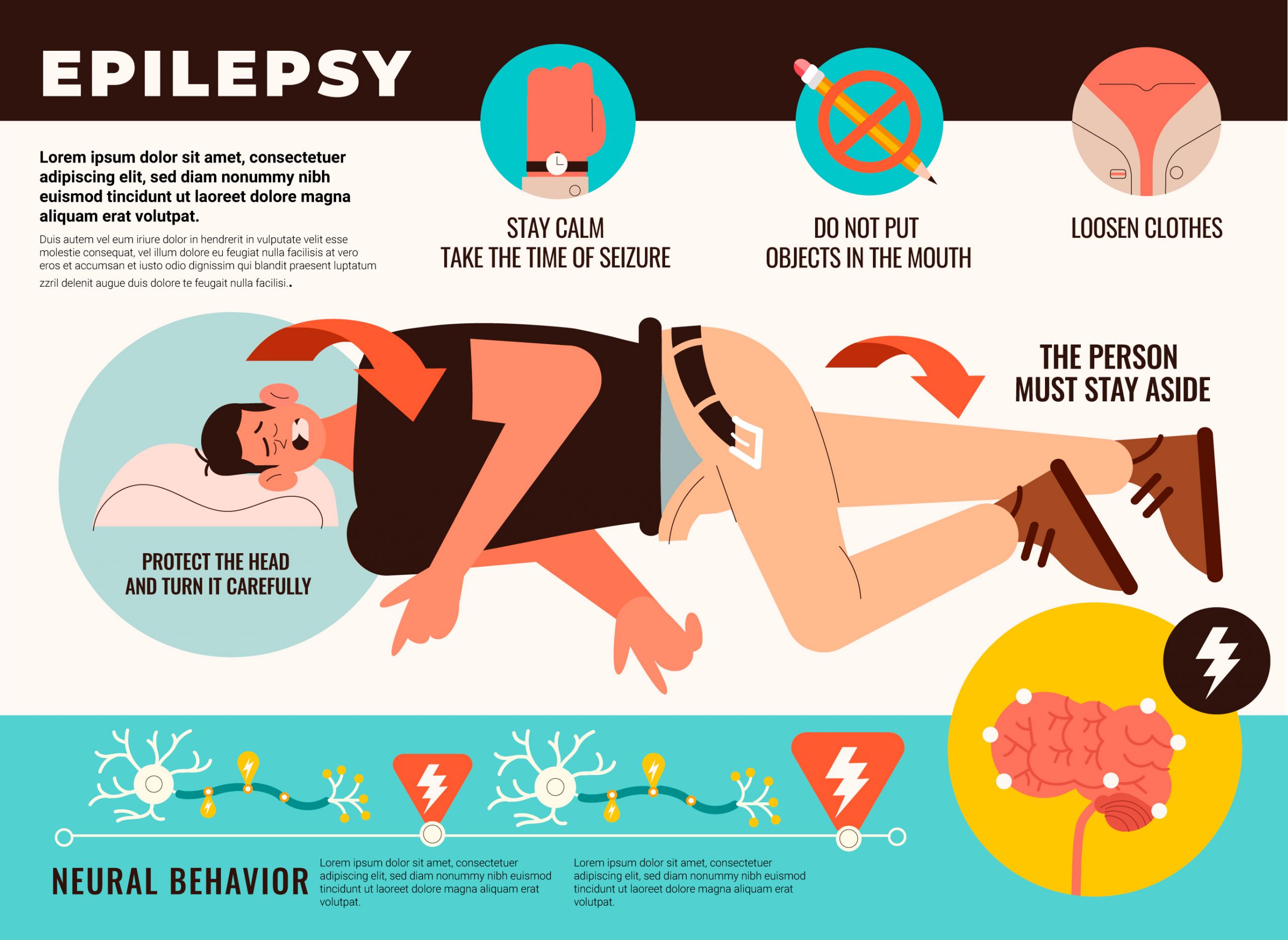
The first approach in a child presenting with status epilepticus or seizures, should focus on airway management and adequate ventilation and circulation. It is important to safeguard patients from injuries caused by involuntary motor activities. It is also important to place the patient in a lateral position to prevent aspiration and position a peripheral venous catheter. Vital signs (heart rate, blood pressure, oxygen saturation, and temperature) need to be monitored. A rapid blood test should be done to recognize hypoglycemia, which is a common cause of seizures in children .
 Benzodiazepines are considered the first choice in the initial treatment of seizures and SE in pre-hospital emergency care. They increase inhibition of GABA receptors, have a rapid onset and are effective in 79% of patients in status epilepticus . Barbiturates increase inhibition of GABA receptors.
Benzodiazepines are considered the first choice in the initial treatment of seizures and SE in pre-hospital emergency care. They increase inhibition of GABA receptors, have a rapid onset and are effective in 79% of patients in status epilepticus . Barbiturates increase inhibition of GABA receptors.
Phenobarbital and Phenytoin are considered second-class drugs to treat seizures and SE, and they are usually administrated when benzodiazepines fail. Side effects are: sedation, respiratory depression, and hypotension. So, airway management and cardiovascular treatment should be considered as priority. Valproic acid is important in refractory SE.
What are points about which the parents need to be counselled?
Parental counselling sessions must be an essential part of the management of first seizure in children in order to allay parental fears, negative reactions, and apprehensions of stigma or social taboo. The main focus of discussion with parents may include the chances of its recurrence, home management of seizure, need for AEDs, possible adverse effects of AED, duration of AED therapy, role of investigations techniques such as MRI brain and EEG, and based on the etiology explanation of overall outcome of seizure. Domiciliary management of seizure must focus on emphasis of recovery position during active seizure and use of rescue medication such as intranasal midazolam (0.2 mg/kg; maximum: 10 mg) in case of prolonged seizure (>3-5 min). In addition, parents must be counselled to maintain strict compliance with medications, need to administer medications by correct measurement (using syringe for mL) and to report to treating physician in case of any adverse event or seizure recurrence. In this regard, it will be useful to give these instructions as a patient information sheet.

What is the mortality rate in children with epilepsy?
The mortality rate in people affected by epilepsy is 2–4 times higher than the rest of the population, and 5–10 times higher in children [19]. Early death risk in children without neurological comorbidity is similar to the general population and lots of deaths are not related to seizures themselves but to the neurological pre-existing disability. Sudden unexpected death in epilepsy (SUDEP) represents the most common cause of death related to epilepsy in children. Global mortality rates are between 2.7 and 6.9 death per 1000 children every year; SUDEP related mortality in children is about 1.1–2 cases/10,000 children per year.
Key Messages
- Childhood seizures and status epilepticusrequire early and effective treatment.
- Long term outcomes are better in children with epilepsy, if anti-seizure medicationsare initiated early.
- Domiciliary care is very important and parents of children with epilepsy need to be educated about it.
- Parents and children need to be counselled regarding the do’s and don’ts, that needs to be followed in children suffering with epilepsy.
For further information, parents may log on to www.pedneuroaiims.org and click on the “Parents Corner” Tab to know more about Childhood Epilepsy in children, Febrile Seizures and domiciliary care of seizures at home.

An Epilepsy Module Handout was released in March 2022, in collaboration with Academy of Pediatric Neurology, Indian Academy of Pediatrics (IAP) and IAP Aligarh and Dehradun branches, containing the summary of webinars of various childhood epilepsies. You can scan the QR code given below to gain access to the various You Tube links, of the various webinars.
The revised guideline on the management of Childhood Epilepsy was launched in September 2022, at Srinagar, in collaboration with the Academy of Pediatric Neurology, Indian Acdemy of Pediatrics.
(The authors are from Centre of Excellence and Advanced Research for Childhood Neurodevelopment Disorders, Child Neurology Division, Department of Pediatrics, AIIMS, New Delhi)

