Covid-19 in Children
In present scenario the Coronavirus disease 2019 (COVID-19) pandemic caused by the severe acute respiratory syndrome Coronavirus 2 (SARSCoV-2) is the ongoing global public health crisis leading to many deaths. In India, the first case of COVID-19 infections was reported in Kerala on January 27, 2020. Subsequently the case load increased steadily leading to a peak case load of nearly one lakh new cases per day in the month of September 2020…..
By Dr. Neelam Mohan/ Dr Sailen Kumar Bana
The daily case load subsequently decreased. Nearly 6 months after peaking of cases in first wave in September 2020, coronavirus cases in India once again started rising from the first week of March 2021, heralding the arrival of second wave of COVID in the country. As per the Lancet editorial April 2021, due to premature reduction of our guards in terms of covid appropriate behaviour associated with super-spreader events like political rallies and religious gatherings led to a massive surge of cases in 2nd wave. As on 10th of May 2021, the health ministry reported 366,161 new Covid-19 infections and 3754 more deaths. India’s total caseload now stands at 22.66 million, with 246116 deaths.
Are the coronavirus variants more infectious in 2nd wave?
The second wave of the pandemic has started gripping the country since first week of March 2021. India has also reported many mutant stains of coronavirus causing an increase in the number of COVID-19 cases in the country. Double mutant strain (B.1.617 variant) is the predominant variant in 2nd wave in India, which has been declared as variant of concern by WHO due to its association with increased transmissibility and detrimental changes in COVID-19 epidemiology. Other stains are Bengal strain (B.1.168), UK Strain (B.1.1.7 Variant), South African Strain (B.1.351 Variant),Brazilian Strain (P.1 Variant). B.1.618 is a new lineage of SARC-CoV-2 characterized by a distinct set of genetic variant including E484K, which has immune escape mechanism, which means that previously formed antibodies against a virus without this mutation may be less effective in inhibiting this virus strain.
 Are Children being more affected in 2nd wave of Covid-19?
Are Children being more affected in 2nd wave of Covid-19?
More children are being affected in this wave, though many of them present with mild symptoms. In the first wave, pediatric patients attributed to 2.8 % of the total cases. In the 2nd wave, nearly 11.5% of the 56 lakh Covid-19 cases reported between January 1 and April 21 were in the age group zero to 20 years.
What are the symptoms of COVID in children?
The infection course in children is milder compared to adults. The reasons behind milder course in children are due to decreased expression of ACE inhibitor-2 receptor in children, decreased immune response and interference by other coinfecting viruses, stronger innate immune response, higherproportion of total lymphocytes, absolute numbers of T and B and NK cells and lower pro inflammatory cytokine responses. Symptoms and signs of COVID-19 are nonspecific and resemble any viral illness. Few common symptoms like in adults are fever, headache, myalgia, fatigue, tiredness, coryza, cough, sore throat, rapid breathing, loss of smell and taste. Children more commonly present with diarrhea, vomiting, abdominal pain, poor feeding. Patients may remain asymptomatic despite being infected.
 Can children be super spreaders?
Can children be super spreaders?
A super spreader is a person infected with the SARS-CoV-2 virus who is able to transmit the virus to a disproportionately high number of people.According to a study published in JAMA, children the viral load in the nasopharynx and oropharynx of children is 10 times higher as compared to adults, though they may have mild or no symptoms. Children usually mix around the adults, and more often visit their grandparents. This increased load of the virus in children may cause more droplet spread to the people who take care of them or come near to them without following COVID appropriate behavior.
Should children be tested?
To avoid transmission to other household members, testing is recommended for all the suspect cases however, if resources are scarce, then testing may be deferred for both asymptomatic contacts and children with mild symptoms and without any comorbidities and a known positive family member. Such children may be presumed to be infected and they should be managed as per the guidelines. Presently in India, we do not have scarcity of resources so it it advised to test them to isolate the patient and prevent spread to others.
What test should be done to diagnose Covid-19 infection?
Patients should undergo testing as soon as possible after onset of symptoms. Rapid Antigen Test in nasopharyngeal swabs has low sensitivity, so if negative, RT-PCR should be done, which has a sensitivity of nearly 70% if done in nasopharyngeal and oropharyngeal swabs. Other tests like Xpert SARS-CoV-2 and Truenat give faster results. The Xpert Xpress SARS-CoV-2 test is a rapid, real-time RT-PCR test intended for the qualitative detection of nucleic acid from the SARS-CoV-2 in upper respiratory specimens. TrueNat system is a multiplexed point of care test that includes a single assay comprising of both the screening (E gene) and confirmatory (Orf1a) targets in a single test.
Who are high risk children in India?
Children with chronic illnesseslike diabetes, asthma, obesity, sickle cell disease, malignancy on immunosuppressive therapy, post organ transplantation (renal , liver , bone marrow ), immunodeficiency disorders like HIV, genetic, neurologic, metabolic conditions are considered high risk. These patients may manifest with severe symptoms and need good supervision and timely management.
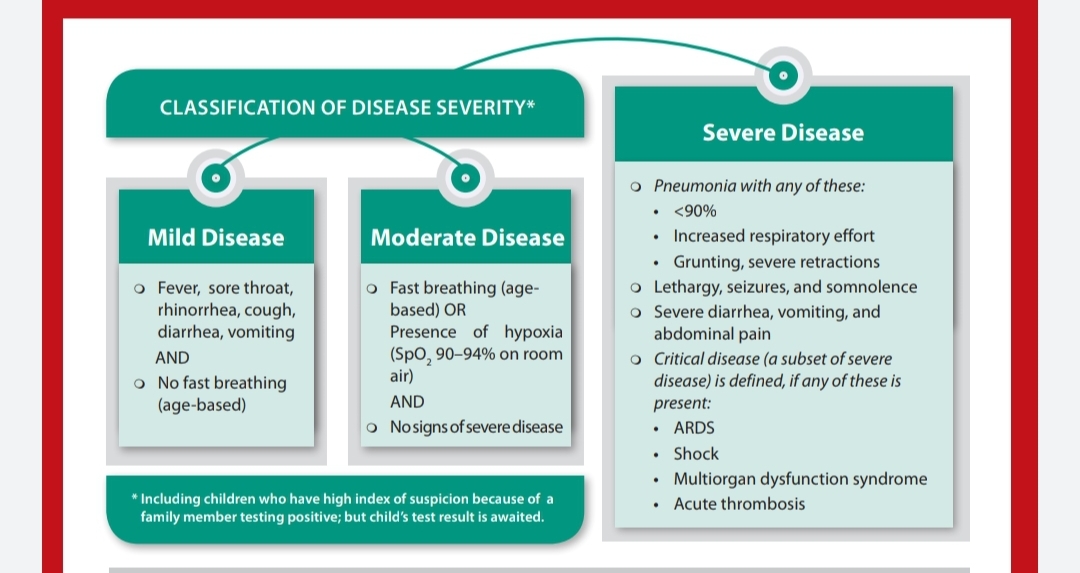
What is the severity grading of Covid in children? Where and how to treat them?
Affected children are graded as mild/moderate/ severe cases according to their symptoms and the treatment protocol differs accordingly.
Mild disease: Children with mild disease present with fever, cough, rhinorrhea, diarrhea, vomiting without fast breathing.Children with mild symptoms may be managed at home. Adequate hydration and nutrition is to be given. Temperature and oxygen saturation level has to be monitored every 6 hourly. Paracetamol is to be used in case of fever. Strict monitoring of patients and regular supervision by health care personnel by tele consultation is required to look for the danger signs and identify the progression of mild cases to moderate or severe disease.
 What are the danger signs which should warrant immediate medical attention?
What are the danger signs which should warrant immediate medical attention?
SpO2 levels falls below 94%
Patient is breathless or develops bluish discoloration
RR >50 in less than 1 year children ; >40 in 2-5 yrs ; and >30 in >5 yrs
Blood in sputum
Altered behavior or confusional state/lethargy
Not accepting feed and decreased urine output
Excessive vomiting or diarrhea with dehydration
Moderate disease: Children with moderate disease present with fast breathing and / or hypoxia (saturation between 90 % to 95%). These children need to be admitted in COVID ward. Some tests like CBC, LFT,RFT,CRP, X-ray chest needs to be done. Adequate hydration has to be ensured. Fever is to be controlled with Paracetamol. If saturation is less than 94 %, and the disease is rapidly progressive, then injections like remdesivir, methylprednisolone, antibiotics may be required. Amoxycillin to be used with suspicion of bacterial infection. Prone positioning during awake period improves oxygenation. Supplemental oxygen is required if saturation is below 94 %.
Severe disease: Children with severe disease present with pneumonia with saturation below 90 % in room air, increased respiratory effort, grunting /retraction, lethargy, seizures, and somnolence, severe diarrhea, vomiting or abdominal pain. These children need ICU care, and should be assessed for thrombosis and hemophagocytosis. Investigations like CBC, CRP, procalcitonin, LFT, RFT, D-Dimer, ABG, lactate, ferrititn, LDH, echocardiography , X-ray chest should be done. These children require oxygen support by high flow nasal cannula/ pressurized oxygen through CPAP/ Ventilator. They require intravenous antibiotics, remdesivir, steroids (dexamethasone), anticoagulant like enoxaparine. Unlike adults, the role CT thorax is limitedin children. CT thorax is indicated, if any additional lungs pathology is anticipated, or if RT PCR is negative but the patient is symptomatic in the form of respiratory distress and hypoxia.
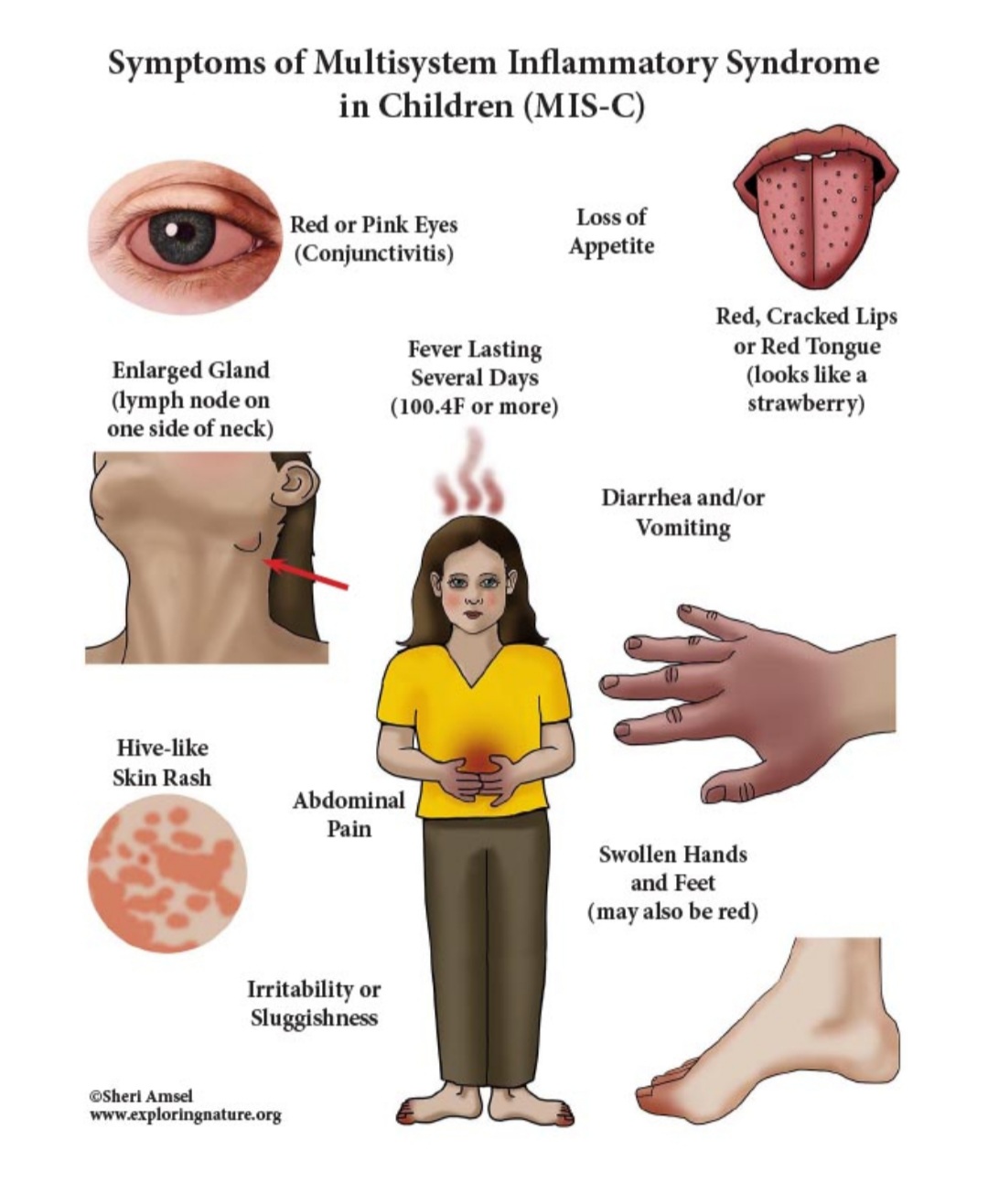
Multisystem inflammatory syndrome in children (MIS-C):
It is a serious illness in children affecting multiple organ system that seems to be related to COVID-19. It appears to be a delayed complication of coronavirus infection, although not all children with MIS-C-related symptoms test positive for the virus. MISC is caused by a delayed immune response to the coronavirus that somehow goes into overdrive, causing inflammation that damages organs. It’s also possible that the antibodies children make to the virus are creating the immune reaction. Since only a small number of children develop MIS-C, it is possible that there are genetic factors that make some children susceptible. MIS-C has varied symptoms that affect several organs and systems in the body. The usual duration between acute infection and onset of MIS-C symptoms is two to six weeks. However, rare cases of MIS-C occurring beyond 6 weeks after the acute SARS-CoV-2 infection have been reported. Fever is the prominent symptom. In contrast to the WHO, the CDC case definition permits a shorter duration of fever (> 24 h versus>3 days). Many children have symptoms like body rash, conjunctivitis, symptoms resembling toxic shock syndrome or Kawasaki disease, in which blood vessels, including the coronary arteries, enlarge or form aneurysms. Some children have signs of excessive blood clotting, gastrointestinal symptoms, kidney injury, neurologic symptoms, or heart inflammation with impaired heart function. These symptoms can occur in different combination. Once MIS-C is diagnosed, children will need to be followed over time with laboratory tests to assess inflammation, blood clotting, liver function, heart function, and other aspects of their illness. Children should also have echocardiograms to evaluate their heart and coronary arteries. Treatment currently includes anticoagulation to curb blood clotting, IV immunoglobulin, and anti-inflammatory drugs (corticosteroids and drugs blocking IL-1 or IL-6).
 Covid Vaccination in Children:
Covid Vaccination in Children:
Though most children are at low risk for complication, the need for a pediatric vaccine may not seem pressing, but this pandemic may never be controlled if children are not vaccinated, because they may act as silent carrier. There is increased recognition of MIS-Cand children with risk factors (chronic lung disease, heart disease, liver and kidney disease) are at increased risk for complications. So, once the safety and efficacy of vaccines in children are proved, they should undergo vaccination. Presently, many vaccines are under trial across the globe. Pfizer vaccine, a mRNA vaccine has been approved for use in children between 12 to 18 years in US and Canada. Moderna vaccine also a mRNA vaccine is conducting two separate trials for children in USA aged 12 to 17 years and for children 6 months to 12 years, and the initial data shows that, it is 96% effective for adolescents between 12 to 17 years, without any safety concern. Bharat Biotech Covaxin. Recently it has got a nod from DCGI for trials in children aged 2 years-18years.
Psychological Impact on Children
India has the largest child population in the world with children below the age of 20 years constituting almost 41% of the total population of 136 crores. The lockdown has significantly impacted children from poor families. An increasing number of poor and street children now have no source of income, making them a high risk population to face abuse and mental health issues with greater vulnerability and exposure to unfavorable economic, social and environmental circumstances.
The home confinement of children and adolescents is associated with uncertainty and anxiety which is attributable to disruption in their education, physical activities and opportunities for socialization with peer group.There is increased use of internet and social media among adolescents, which predisposes them to access objectionable content and also increases their vulnerability for getting bullied or abused. Children are also experiencing disturbed sleep, nightmares, poor appetite, overeating,agitation, inattention clinging and separation related anxiety.
There is a need to improve the infrastructure for children and adolescent’s access to mental health services by using both face to face as well as digital platforms. For this collaborative network of parents, psychiatrists, psychologists, paediatricians, community volunteers, and NGOs are required. There is a need for ‘tele mental health compatibility’ and be accessible to the public at large. This would be crucial to prevent during and post-pandemic mental challenge.
Role of parents
In the times of stress and uncertainty, a secure family environment which the parents can provide is a strong protective factor. There is evidence to show that parental practices and coping measures affect the children’s post disaster mental health. Parents should spend the undivided quality time with their kids and should not transfer their own fear and anxiety. Children should be put on a set routine and parents should promote the healthy and balanced diet, maintain oral health, physical exercise, proper rest, avoidance of fatigue.

Routine vaccination in children during pandemic
As per the guideline formulated by Ministry of Health and Family Welfare (MOHFW), India, routine vaccination of children should not be disrupted during the pandemic. A health facility should continue immunization services with below mentioned prerequisite arrangements:
- A well-ventilated seating area with seating arrangements done as per the social distancing norms. The vaccine should preferably be called by appointment although no opportunity should be missed for vaccination.
- An adequate number of pre-identified, fixed vaccination staff depending on the injection load and the required documentation.
- Staff conducting vaccination should wear a three-layered surgical mask and gloves and sanitize their hands after vaccinating every child.
- Support staff to manage seating arrangement, queue management etc. for the pregnant women and care givers.
- Ensure hand sanitizer or hand washing units with chlorinated water are available for public use at the entrance to the health facility
- Disinfect the seating space after completion of the immunization session.
- Adequate availability of MCP card and due updating of records.
- Adequate availability of vaccines and logistics for the uninterrupted immunization session
- Display visual alerts in clinics, such as posters, with information about COVID-19 disease and reminders on individual prevention strategies.
Can mothers with Covid breastfeed their babies?
Neonates can acquire Covid 19 during delivery, but more commonly during postnatal period at home, however, majority of them are preventable. If the mother is stable clinically, then roomin, breast feeding, kangaroo mother care, immunization and routine care should continue. Mothers should perform hand hygiene frequently, including before and after breast feeding and touching the baby. They should practice respiratory hygiene and wear a mask while breast feeding and providing care to the baby. Cleaning and disinfecting the surfaces should be done regularly
Mucormycosis – Is it an entity to worry about?
In the absence of an effective vaccine or antiviral therapy, glucocorticoids and probably remdesivir are the only drugs proven to be beneficial in Covid-19. Glucocorticoids can increase the risk of secondary infections. Moreover, the immune dysregulation caused by the virus and the use of concurrent immunomodulatory drugs such as tocilizumab could further increase the risk of infections in COVID-19 patients.
Infection with mucormycosis, known as the black fungus, is a dangerous fungal infection caused by a group of moulds known as mucormycetes, which are present naturally in the environment, but they cause serious complications when a patient has pre-existing health problems or has received steroids.
In Covid-19 patients with diabetes and immuno-suppressed individuals, one must suspect mucormycosis if there is sinusitis, nasal blockage or congestion, one-side facial pain or numbness, blackish discoloration over the bridge of the nose or palate, toothache, double vision with pain, skin lesion, thrombosis, chest pain and worsening respiratory symptoms.
Mucormycosis is treated by antifungal drugs like Amhotericin B, posaconazone, however, extensive debridement might also be required.
Threat of 3rd Wave—is it inevitable in India?
There is high possibility of a 3rd wave in India somewhere between October – December 2021. The 3rd wave can only be prevented with rapid vaccination, stringent government action to make people follow the COVID appropriate behaviour along with early identification of mutant stains. In the third wave, there will be only children who have not been vaccinated so far, as the inoculation drive for those below 18 years has not started yet. So, children will be more vulnerable to be affected by COVID in 3rd wave. There is deficit of with special paediatric ICU beds, which have to be increased as a preparedness for the future wave along with the need of training doctors nurses and other healthcare workers for good pediatric care. Need for a special pediatric task force both at national and state level cannot be under emphasized.
(The authors are Director, Department of Pediatric Gastroenterology & Hepatology/ Lead Pediatric Covid Care, Medanta TheMedicity, Gurugram)

