Lighting up Lives
Chief of the prestigious RP Centre for Ophthalmic Sciences, AIIMS, New Delhi, Dr Atul Kumar has pioneered modern Vitreous Retinal Surgery that has emerged as a ray of hope for preventing irreversible blindness due to Diabetic Retinopathy. Double Helical takes a close look at the inspiring life story of the eminent doctor who has scaled the pinnacle of medical excellence through sheer grit, guts and gumption
It was a long and arduous journey for young Atul who came from a non-medico family background and struggled against all odds to get a meritorious seat at Maulana Azad Medical College, Delhi. Today, as Chief of the RP Centre for Ophthalmic Sciences, AIIMS, New Delhi, a premier institution in the field of eye care, Dr Atul Kumar has achieved global recognition as a top-rated Vitreoretinal Surgeon. He attributes the fame he has achieved for medical excellence to his passion to serve the patients who come to him from all over the country and the world.
His current routine involves teaching post-graduates at the renowned eye institute (RP Centre runs among the largest residency programs anywhere in the world, with over 130 residents doing MD at any point of time). Besides this, Research and Thesis guidance is also an integral part of the faculty curriculum. He handles the heavy clinical load with the-state-of-the-art labs including the Retina Lab equipped with high-tech, sophisticated imaging equipment to help diagnose retinal diseases. As Dr Kumar says, name the newer equipment and we have it.
R P Centre, which he heads, has an astounding 16 operation theatres or operating rooms (ORs) where various ocular and orbital surgeries are performed round the clock. The centre also boasts of a 24×7 huge casualty manned by consultants and residents who take care of eye ailments or injuries etc any time of the day or night, and perform surgery immediately, if required. A non-profit organization under the Ministry of Health and Family Welfare, it is affordable to all segments of the society.
MEDICAL JOURNEY & MILESTONES
Dr Kumar completed his MBBS from the famed Maulana Azad Medical College in 1980 and joined as an MD resident at the RP Centre soon after. He rose by dint of his merits to become a senior resident and then became a part of the Faculty as Assistant Professor at the same Institute. In 1990 he left for doing a retinal training from the University of Maryland at Baltimore, USA. On his return he adopted many techniques to improve standards and outcomes of retinal surgery which resulted in an extremely high rate of success at the Centre.
He rose through his faculty promotions and is now a Professor in the Vitreoretinal Service at the RP Centre. As Chief of this premier wing, he has managed to streamline the academic program for both senior and junior residents involving them in research and teaching besides their clinical work. He has also helped in improving the infrastructure at the eye centre and it now matches any private centres when it comes to the interiors. The latest equipment and skilled doctors have now made RPC stand among the finest eye institutes in the world. His moment of glory recently came when the WHO acknowledged RP Centre as a collaborating centre for Prevention of Blindness in September 2016.
Publications:
Dr Atul Kumar has over 218 indexed and non-indexed publications to his credit and about 24 book chapters which he has written for various books.
Diabetic Retinal Blindness: Dr Atul Kumar’s Viewpoint
Diabetes mellitus is an important public health problem. The WHO estimates suggest that there are 422 million people living with diabetes globally, which is about 8.5% of the world adult population. It is also estimated that over 1 million deaths annually are attributed to elevated blood sugar and about 12% of global health expenditure is spent on treatment or prevention of diabetes and its related complications.
Prevalence of diabetes is growing in pandemic proportions. Between 1980 and 2015, there has been near doubling of the prevalence of diabetes from about 4.7% to the current 8.5%. In addition, there are over 300 million people with impaired glucose tolerance, more than half of who will turn into diabetic. A disease that was once considered a “rich man’s disease” is now seen almost in similar proportions in high, middle and low income countries with currently about three fourth of all the diabetics in the world residing in a low or a middle income country.
India was once called the “diabetes capital of the world”, till it was overtaken by China a few years ago. Nevertheless, we have the second largest diabetic population in the world – an estimated 69 million people. This is expected to rise to about 120 million by 2040. An additional 77 million people are prediabetic which places them in imminent danger of being affected by diabetes. About 1 in every 10 persons above 20 years of age in India has diabetes and the most tragic bit of the data is that more than 50% of them are unaware of their disease and are at a very high risk of developing one of the complications of diabetes. Studies from south India indicate that one in every 5 adult living in urban areas has diabetes.
Morbidity in diabetes is primarily through one or more of its complications like nephropathy, retinopathy, heart disease, peripheral neuropathy or foot disease. Diabetic retinopathy (DR), much like how diabetes affects elsewhere, affects the microvasculature of the retina leading to capillary closure, damage to blood retinal barrier, retinal ischemia, subsequent fibro vascular proliferation and vision loss that can be profound, irreversible and bilateral.
DR is the cause of 1.9% of moderate or severe visual impairment globally and 2.6% of blindness. WHO recognises DR as one of the priority eye diseases that require urgent attention from health care professionals, health organizations and Governments. One in every 3 adults over 40 years with diabetes was found to have DR in the west. Studies suggest that prevalence of retinopathy in persons with diabetes is 35% of which 1/5th of them are in imminent danger of severe vision loss. One out of every five people with diabetes in India has some degree of DR and an estimated 6 million have the severe, sight threatening form called the vision threatening diabetic retinopathy.
Diabetic Macular Edema
Diabetic retinopathy progresses from an innocuous non-proliferative stage, over years and sometimes decades, to the more ominous proliferative stage that requires treatment. Diabetic maculopathy can occur during any of these stages, more frequently seen in the advanced stages and also requires treatment. The unfortunate face about this, though, is that DR is mostly asymptomatic throughout the course till a proliferative disease bleeds into the vitreous cavity or till the maculopathy appears. The fortunate side of the same fact is that it gives ample opportunity for health care professionals to screen, refer and appropriately manage cases of DR before vision threatening forms of DR develop. Diagnosis of even non-proliferative stages of DR mandates advice on strict metabolic control and frequent follow up to monitor progression and need for treatment.
Multiple large scale epidemiological studies from the west and India have shown that duration of diabetes is the single most important risk factor for the development and progression of DR. The longer a patient has diabetes, the more likely he is to have DR and the more likely he is to also have the vision threatening forms of DR. Along with the duration, other important risk factors include the glycemic control, other co-morbidities like hypertension, dyslipidemia, nephropathy, anaemia, genetic factors etc. Except for the genetic factors, all of the above risk factors are modifiable and it has been shown in multiple prospective cohort studies that control of these parameters can help in prevention and slowing progression of diabetic retinopathy.

DR primarily affects patients of working age group causing tremendous personal and social economic strains. Western data suggests that the annual cost per patient with diabetic maculopathy is approximately twice as high as those of patients with diabetes alone. Additionally, the patient will bear non-medical costs of outpatient visits, nursing care and non-medical therapies. There is limited data on the economic impact of DR in India but it is likely to be significant and growing. A more worrisome fact is that increasingly diabetes is being diagnosed at younger age group and these youngsters with early onset diabetes are showing almost two times increased prevalence of DR.
Treatment of diabetes mellitus is simple in earlier stages where all it requires to be done is metabolic optimization of patient, good dietary advice, change in life-style and a regular follow up. But as disease progresses, treatment becomes more protracted, more expensive and less effective. Diabetic maculopathy is the most common cause of any vision loss in patients with DR and currently intravitreal injections of anti-vascular endothelial growth factors are the first line of treatment for this condition. Although effective, this treatment is expensive, invasive, requires multiple and repeated visits and is difficult to sustain in resource limited setting. Other options available are intravitreal injections of steroids and laser photocoagulation. In contrast, gold standard in the treatment of proliferative DR remains laser photocoagulation. In advanced cases of proliferative DR and maculopathy, vitrectomy may be necessary. These treatments require special skills on the part of the ophthalmologist, advanced instrumentation and modern machinery. With growing DR prevalence, these needs are expected to strain the existing eye care systems.
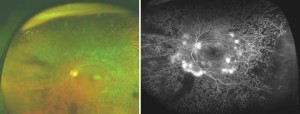
PDR with peripheral ischemia on Ultra-Wide Field Imaging (OPTOS 200)
Over the last decade there has been a keen interest in the genetic make-up of the “Asian-Indian phenotype” that predisposes south Asians to diabetes. But any discussion on this should not undermine the fact that diabetes is indeed a life-style disease and that with increased sedentary and westernized life style, the prevalence of diabetes is increasing by the year.
Type-2 diabetes is a largely preventable disease. Simple measures targeting dietary habits and sedentary lifestyle have been shown to go a long way in preventing diabetes and ensuring a general cardiovascular wellbeing. In this regard, working with the civil society and a policy change at the government level for appropriate environmental changes are necessary. Organizations like the International Diabetes Foundation advocate a multitude of measures ranging from a ban on sponsorship of sporting events by manufacturers of sugar-sweetened beverages and high sugar foods to tax incentives to reduce consumption of sugar sweetened beverages and high sugar foods.
In patients with diabetes, retinopathy is preventable. Good and sustained diabetes control has been shown in multiple large studies like the DCCT, UKPDS and ACCORD to prevent and delay appearance and progression of DR. Other associated risk factors that worsen DR also need to be well controlled and our colleagues in internal medicine, endocrinology, nephrology and cardiovascular medicine play a crucial role in this. Also, since one of them is likely to be the first contact and long term care giver for patients with diabetes, it is his/her responsibility to sensitize patients for need for regular ophthalmic check-up and to provide timely referral. To provide a comprehensive care to the patient with diabetes by a team that includes an endocrinologist, nephrologist, ophthalmologist, cardiovascular physician, neurologist, podiatrist and a dietician is every doctor’s duty towards his patients. If DR does occur in spite of all of these efforts, blindness is also preventable. Early detection and timely treatment of DR has shown to reduce the risk of disease progressing to blindness by over 90%.
The backbone for any preventive program for DR is the screening of patients with diabetes for DR. While use of direct ophthalmoscopy in all diabetic patients need to be encouraged among physicians and diabetologists, often these examinations do not reach sufficient sensitivity and specificity for adequate diabetic screening and referral to an ophthalmologist for a slit lamp biomicroscopy or fundus photography for the screening of DR is necessary. Recently, telemedicine in the screening has shown promise in terms of sensitivity and specificity, scale of application, documentation and ease of non-mydriatic examination.
Simultaneously, efforts need to be made towards increasing awareness among the public, nurses, health workers and even among physician colleagues about need for regular screening and the effects of late diagnosis of advanced stages of DR. In this light, it is a welcome step that DR is included under comprehensive eye care in the national program for control of blindness. With about 69 million diabetics in the country and about 11500 ophthalmologists, every ophthalmologist is required to screen at least 17 diabetic patients every day even if only an annual screening is considered necessary for all of them. Clearly, this is a target that is still far from being achieved!