Restoring Young Lives
Living related pediatric liver transplantation has gained popularity in Eastern countries such as Japan, Korea and India but the procedure is quite challenging and requires specialized care…
By Dr Neelam Mohan

Liver transplantation or hepatic transplantation is the replacement of a diseased liver with a healthy liver allograft. The most commonly used technique is orthotopic transplantation, in which the native liver is removed anad the donor organ is placed in the same anatomic location as the original liver. The history of pediatric liver transplantation (LT) starts with the first human attempt at transplantation by Dr. Starzl in 1963. Since then, new advances and techniques in both surgical and medical management have increased the incidence and improved the outcomes of LTs to >90% survival.
Indications for LT in children
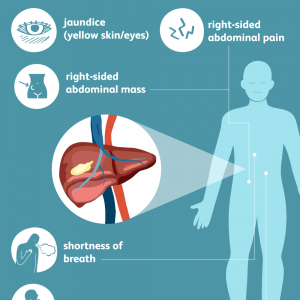
The indications for LT in children have traditionally been
End-stage liver disease with a predicted life expectancy under 1 year
Acute liver failure (ALF)
Unresectable localized hepatic tumours
Liver-based metabolic defects
Other indications include growth failure, intractable pruritus or bone density loss from cholestatic disorders, intractable seizures from metabolic liver disease, and liver tumours in the absence of significant extrahepatic disease. Biliary atresia is the leading diagnose of pediatric liver transplant recipients across the globe.
In liver failure, the decision to proceed with transplantation should be made at a point when there is no clinically significant evidence of liver regeneration or recovery of function. Selection of FHF candidates for transplantation is difficult. The King’s College Hospital criteria have been extensively used and are acknowledged to have a high degree of specificity but have been criticized for lack of sensitivity. More recent recommendation from the same group is to use an INR > 4 or factor V concentration < 25% as the best available criteria for listing for LT. Although these various criteria are helpful, careful observation for progression and clinical change is most rewarding and emergency referral to a transplant centre is of paramount importance.
Liver transplant surgery
The graft is either a cadaveric liver or a living related.
In cadaveric liver transplantation, the liver of a brain dead person is used for transplantation. Cadaveric transplants could be:
Whole graft: The entire graft is transplanted in the recipient.
Reduced graft : When only a part of the cadaveric liver (i.e. right/ left/left lateral part) is used for the recipient
Split graft: The shortage of suitable organs for young children led to development of split livers. The liver of the cadaveric donor is divided and used for two patients usually the right lobe for adults and left lobe for children.
 Living related liver transplantation: This has been a further step to answer the shortage of organs for children. In living related liver transplantation, a part of the liver from a living related donor is used in the child. This procedure is more popular in Eastern countries like Japan, Korea and India where cadaveric liver transplantation has not been possible until recently.
Living related liver transplantation: This has been a further step to answer the shortage of organs for children. In living related liver transplantation, a part of the liver from a living related donor is used in the child. This procedure is more popular in Eastern countries like Japan, Korea and India where cadaveric liver transplantation has not been possible until recently.
Blood group compatible: Mostly blood compatible transplants are done. However in living related liver transplant scenarios recently ABO incompatible transplants are also being done with pre-operative use of plasmapheresis and modified immunosuppression.
Immunosuppression: Following liver transplant, the patient requires immunosuppression usually for whole life according to the present consensus. The most common immunosuppressive drugs used following liver transplantation are tacrolimus, mycophenolate mofetil and steroids. Few centres use steroids sparing induction regimen with Basiliximab. Newer drugs like OKT3, sirolimus and everolimus are used in occasional patients.
Postoperative complications
Early postoperative complication includes primary graft non-function, surgical complications, vascular thrombosis, and venous outflow obstruction, rejection, biliary complications sepsis.
Late complications post-transplant fall into two general categories: (1) Complication related to allograft itself and (2) those related to immunosuppressive drugs. They include chronic rejection, CMV and EBV infection, late biliary strictures, hepatic artery or portal vein thrombosis, post-transplant lymphoproliferative disease (PTLD), De novo auto immune hepatitis, graft fibrosis, Nephrotoxicity and hyperlipidemia secondary to immunosuppressive drugs.
Outcome
Outcome of paediatric liver transplantation has shown incremental improvements from the 1980s to late 1990s. Better management of immunosuppression have not only increased survival rates that are currently reported as 95% at 1 year and 80-90% at 10 years but have also improved quality of life after transplant.
Quality of life
It is now anticipated that children who survive liver transplant will achieve a normal lifestyle despite the necessity for continuous monitoring of immunosuppressive treatment. An important aspect of long term survival is the development of puberty.
Scenarios of Liver Transplant in India
In India, predominantly living related liver transplants are carried out. India needs approximately 22/million liver transplants while one per million liver transplants (approx… 1750 transplant in 2017) are being done. The pediatric liver transplants especially of small babies are definitely quite challenging and require specialised care. There are limited dedicated pediatric liver transplant centres available in India with good outcome. Cost of paediatric liver transplant is approximately Rs 15-18 lakh. For those who belong to disadvantaged sections, support group and funds are arranged.
Author’s profile:
Our team has performed 300 paediatric liver transplants of the total 3000 living related liver transplants, 45% indications were cholestasis, 23% of acute liver failure and 31% for metabolic. 195 were male and age ranged from 2.1 kg to 66 kg and mean follow up was 46 (1 month – 14 years). Overall surgical success rate was 95% and 5 years actuarial survival is 90%. Our team is credited with the following:
Global level credits
Word’s successful liver transplant in lightest baby of 2.1kg (2016).
World’s first chain of 3 pediatric living-related liver transplants with 2 donors (2011)
World’s first living related liver transplant that cured a baby with factor VII deficiency (2010)
World’s youngest domino liver transplant (2009)
National level credits:
India’s first successful pediatric cadaveric reduced liver transplant (2003)
India’s first successful survival of liver transplant in a fulminant liver failure (2004)
South Asia’s first successful combined liver and kidney transplant from two live donors (2007)
India’s first successful pediatric liver transplantation with very severe hepatopulmonary syndrome (2016).
India’s first swap liver transplantation (2009)
India’s first ABO-incompatible liver transplant in a child. (2012)
(The author is Director, Department of Pediatric Gastroenterology, Hepatology and Liver Transplantation, Medanta Medicity, Gurgaon)