From Glucose to Wellness
In recent years, a surge of scientific discoveries, nutritional insights, and technological innovations has redefined how clinicians view and treat Type 2 Diabetes. The shift is profound: from simply lowering glucose to protecting organs, improving metabolic fitness, and achieving whole-body wellness. The convergence of medicine, diet, exercise, and technology has made diabetes management not just more effective, but more holistic and humane.
By Dr Anoop Misra & Bhavya Arora

Diabetes management has changed more in the last few years than in the previous few decades. Earlier, treatment relied mainly on two oral medicines (metformin and sulfonylureas) and basic insulins (Regular and NPH). Today, care is far more advanced. Newer diets—such as low-GI (low glycaemic index), high-fibre, and high-protein plans—emerging from a deeper understanding of physiology, help achieve better blood sugar control. Evolving exercise concepts, including strength training, daily step targets, and short high-intensity sessions, further improve insulin sensitivity.

Modern medicines such as glucagon-like peptide-1 receptor agonists (GLP-1 RAs; semaglutide, liraglutide, dulaglutide), dual-incretin therapies with glucose-dependent insulinotropic polypeptide (GIP; e.g., tirzepatide), and sodium–glucose co-transporter-2 inhibitors (SGLT2 inhibitors; canagliflozin, dapagliflozin, empagliflozin) not only lower glucose but also aid weight loss and protect the heart and kidneys. Insulins have also evolved, with ultra-rapid formulations, stable long-acting preparations (over 24-hour action), nasal insulin, and once-weekly basal insulin, making life much easier.
Technology has transformed monitoring as well: continuous glucose monitoring (CGM), time-in-range goals, and smart insulin pens now allow more accurate and safer control. This article discusses these advances in detail.
Diet: Reduce Carbohydrates, Increase Protein and Fibre:
High-fibre, low-glycaemic foods and millets are helpful in diabetes as they keep blood sugar stable and prevent sudden spikes after meals. Fibre slows digestion, helps sugar enter the blood gradually, keeps you full longer, and reduces cravings. Millets like sorghum (jowar), pearl millet (bajra), foxtail millet (kangani), and little millet (kutki) are naturally rich in fibre, slow-digesting, and packed with minerals, making them excellent for digestion, weight control, and stable blood sugar. In simple words, these foods help manage diabetes better by improving sugar control, supporting gut health, and helping with weight management.

Along with millets, a plant-based diet further strengthens diabetes control because it is naturally low in saturated fat, high in antioxidants, and rich in plant proteins from lentils, beans, and legumes, which improve insulin sensitivity. Plenty of vegetables, fruits in moderation, nuts, seeds, and whole grains provide vitamins, minerals, and phytonutrients that reduce inflammation, protect the heart and kidneys, and support long-term metabolic health.
Overall, a plant-focused diet reduces insulin resistance, supports weight loss, improves organ protection, and makes diabetes management easier and more holistic.
Focus Beyond Sugar: Blood Pressure &Cholesterol
In diabetes, high blood sugar is only one part of the problem. Most long-term complications like heart attacks, strokes, kidney failure, and vision loss are caused not just by sugar, but by the combination of high blood sugar, high blood pressure (BP), and high cholesterol. These three together damage blood vessels throughout the body. That is why diabetes management focuses strongly on keeping blood pressure normal and lipids (cholesterol levels) controlled. Good control of BP and cholesterol can reduce the risk of heart disease and stroke.
Believe it or not, we save even more lives by keeping a close watch on cholesterol and blood pressure. Taming those numbers is like giving your heart and blood vessels extra bodyguards, helping you stay healthy and strong for the long run!
Protecting Organs & Preventing Complications
Diabetes affects the whole body not just sugar levels. High blood sugar over time can damage important organs like the heart, kidneys, eyes, nerves, and liver. This damage often happens silently, without symptoms in the early stages. If not prevented, it can lead to serious problems such as heart attacks, kidney failure, vision loss, nerve damage, and fatty liver disease (accumulation of fat in liver). New drugs, lifestyle changes, and regular follow-ups help shield these organs from damage.
Think of your organs as a team of superheroes. Our job is to keep each one strong and protected, while also making sure your blood sugar behaves itself. When the whole team is healthy, you feel your best!

Reducing abdominal fat:
Abdominal fat (measured clinically as waist circumference, Figure 1) is not just “extra weight.” It acts like an active organ that releases chemicals causing insulin resistance (works against insulin’s action), inflammation, high blood pressure, and abnormal cholesterol. This makes blood sugar harder to control and increases the risk of heart disease. People with more belly fat often need more medicines, struggle with higher sugars, and develop complications earlier.
When we tame belly fat, we tame most of the trouble it causes! A flatter tummy means a happier heart, smoother sugars, and fewer complications trying to sneak in. Let’s keep that abdominal fat on its best behaviour!

Exercise: Strength Training, Increase Lean Body Mass and Become Fitter
Strength training with resistance bands, weights, squats, or body-weight exercises helps preserve and build muscle (Figure 2), which improves insulin sensitivity. Muscle acts like a “sugar sponge,” helping the body use glucose better. Walking is still useful, but building muscle is now equally important.
Strength training gives you more active muscle, and these muscles gobble up extra sugar like hungry helpers — so alongside walking, keeping your muscles strong is a powerful way to control diabetes!
Reducing fat in liver:
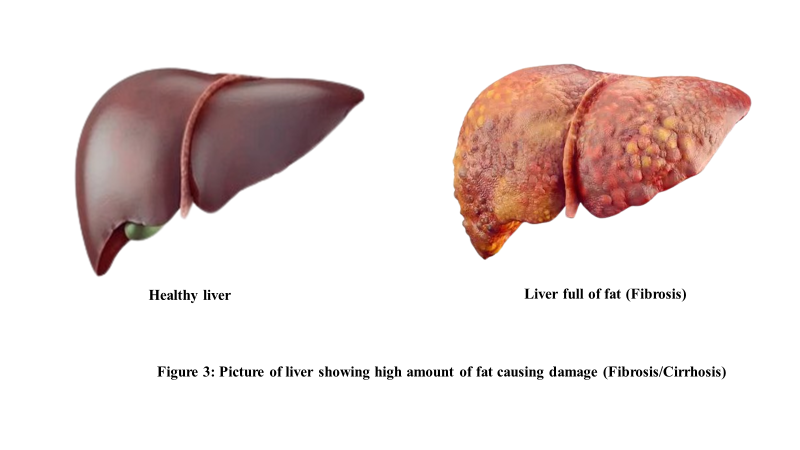
When the liver has too much fat (see Figure 3), it becomes “insulin resistant,” meaning it keeps releasing extra sugar into the blood even when it’s not needed. This leads to higher fasting sugars, more medicines, and greater difficulty losing weight. Excess liver fat also increases the risk of heart disease, inflammation, and eventually liver damage and even cirrhosis. Reducing liver fat improves insulin sensitivity, lowers fasting sugar levels, supports weight loss, and protects long-term liver health.
Newer (Super) Drugs in Diabetes:
Newer diabetes drugs have changed treatment by offering benefits far beyond just lowering sugar. Medicines like:
1. Sodium–Glucose Co-Transporter 2 (SGLT2) inhibitors (empagliflozin, dapagliflozin) work by blocking the SGLT2 protein in the kidneys, which is responsible for reabsorbing sugar back into the bloodstream. When this pathway is inhibited, excess glucose is flushed out through the urine, leading to a natural reduction in blood sugar levels independent of insulin. Beyond sugar control, SGLT2 inhibitors provide strong kidney protection by reducing pressure inside the kidney filters (glomeruli), lowering albumin leakage, and slowing the progression of chronic kidney disease. They also reduce the risk of heart failure by decreasing fluid overload and improving cardiac workload. Overall, SGLT2 inhibitors help control sugar while offering powerful heart and kidney protection.
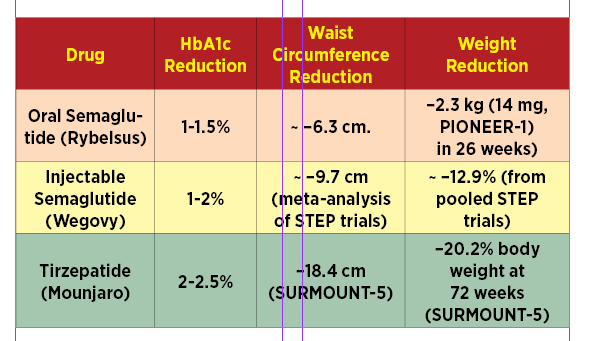
2. Glucagon-like peptide-1 receptor agonists (GLP-1 RAs) (semaglutide, dulaglutide, liraglutide) and drugs acting on glucose-dependent insulinotropic polypeptide (GIP) (tirzepatide) work by mimicking the natural GLP-1 hormone, which increases insulin release when blood sugar rises, reduces glucagon (the hormone that raises sugar), and slows stomach emptying to prevent sugar spikes after meals. The newer dual-action drugs like tirzepatide provide a “double benefit” by activating both GLP-1 and GIP receptors, leading to even stronger effects on blood sugar control, weight loss, and metabolic health. These medications reduce appetite, increase fullness, improve insulin sensitivity, and significantly lower abdominal and liver fat. They also reduce inflammation, improve blood vessel function, and lower blood pressure. Together, these actions protect the heart, decrease the risk of stroke and heart failure, and slow the progression of kidney disease. Table 1shows average reduction in blood sugar (HbA1C), abdominal fat (measured by waist circumference) and body weight in various trial named in capitals.
Table 1 shows average reduction in blood sugar (HbA1C), abdominal fat (measured by waist circumference) and body weight in various trial named in capitals.
Modern diabetes medicines are a real boon — they not only tame sugar, but also look after your heart, kidneys, and waistline all together!
Newer insulins
Newer insulins, like once a day long acting and once-weekly insulins, make treatment simpler with fewer injections. Overall, these advanced medicines make diabetes management easier, safer, and more focused on whole-body protection rather than just sugar control.
What a leap forward — insulin just once a day or even once a week… who could have imagined that years ago!
New Monitoring Technologies: CGM and Time-in-Range
Continuous Glucose Monitors (CGMs) are transforming self-monitoring. These wearable sensors check glucose every few minutes, reducing the need for finger pricks and offering real-time trends, alerts, and insight into how food, exercise, and stress affect sugar levels. They improve time in range and overall control.

However, CGMs are not perfect. They measure interstitial glucose, which may lag behind actual blood glucose, especially after meals, during rapid drops, or during exercise. They can also give occasional inaccurate readings and are more expensive. Therefore, CGMs guide treatment but do not replace finger-prick tests, HbA1c, kidney tests, or cholesterol monitoring.
It feels like magic — glucose numbers all the time without a single prick, but we still need to read them wisely!
Takeaways
Today, diabetes care is no longer just a battle with sugar — it’s a full-body wellness makeover. We now have smart medicines that protect the heart, kidneys, and even the waistline. Food, muscles, and technology have joined the team to keep diabetes on its best behaviour. Care is becoming easier, friendlier, and far more hopeful than before. Now, diabetes isn’t running the show — you are!
(The author is Chairman, Fortis-C-DOC Centre of Excellence for Diabetes, Metabolic Diseases and Endocrinology, Chirag Enclave, New Delhi, Chairman, National Diabetes, Obesity and Cholesterol Foundation (N-DOC), SDA, New Delhi)
With inputs from Bhavya Arora, Clinical Nutritionist & Certified Diabetes Educator, Fortis-C-DOC Centre of Excellence for Diabetes, Metabolic Diseases and Endocrinology, Chirag Enclave, New Delhi.

