One Grain at a Time
 India has made remarkable strides in universal salt iodisation. But with nearly a quarter of the population still lacking access to adequately iodised salt, a robust public–private partnership could be the key to eradicating iodine deficiency.
India has made remarkable strides in universal salt iodisation. But with nearly a quarter of the population still lacking access to adequately iodised salt, a robust public–private partnership could be the key to eradicating iodine deficiency.
By Padma Shri Dr Chandrakant S Pandav
According to the World Health Organization (WHO), iodine deficiency during foetal life and early childhood remains the single most significant, yet entirely preventable, cause of mental retardation across the globe. Even mild iodine deficiency is enough to impair a child’s ability to reach their full intellectual and physical potential.

The sustainable elimination of Iodine Deficiency Disorders (IDD) is directly linked to economic growth. Research shows that the Intelligence Quotient (IQ) scores of children living in iodine-deficient environments are, on average, 13.5 IQ points lower than those living in iodine-sufficient environments. A one-point increase in a nation’s average IQ correlates with a 0.11 per cent increase in Gross Domestic Product (GDP). Therefore, a 13.5-point increase in average IQ could potentially result in a 1.49 per cent rise in GDP — a substantial gain in economic productivity and national prosperity.
Iodine deficiency is fundamentally a disease of the soil. When the soil lacks iodine, the food grown on it is similarly deficient, leading to widespread nutritional gaps. IDDs have been found to be linked to at least 10 of the 17 Sustainable Development Goals (SDGs), including good health and well-being, quality education, and poverty reduction.
Salt, due to its universal consumption and stability, serves as an ideal vehicle for fortification. It is consumed by people across all demographics — rich and poor, male and female, rural and urban, young and old, in all seasons. The average Indian consumes around 12 grams of salt daily, making it an effective medium to deliver iodine.

Under the Universal Salt Iodisation (USI) programme, salt is fortified with iodine to combat iodine deficiency disorders. Since the introduction of USI in India, the country has witnessed remarkable success in its iodisation efforts. According to the India Iodine Survey (2018–2019), iodised salt now reaches 92.4 per cent of the population. USI is regarded as one of the most successful public health interventions globally, playing a crucial role in reducing IDD prevalence worldwide.
The Public–Private Partnership (PPP) Model
Public–Private Partnership (PPP) refers to a collaborative arrangement between the government and the private sector aimed at serving the public good. While the public sector contributes regulatory oversight, infrastructure, and social responsibility, the private sector offers innovation, efficiency, and expertise in delivery and operations. The full potential of the public sector cannot be realised in isolation — it must be complemented by the agility and know-how of private enterprise.
Private sector engagement introduces new opportunities, scalable solutions, and improved quality control, while also helping build accountability into public service delivery. Therefore, a synergistic relationship between the two sectors is vital — especially in health and nutrition programmes like USI.
India has witnessed very few successful PPPs in the health and nutrition domain, but the USI programme stands out as one of the largest and most impactful examples of such collaboration.
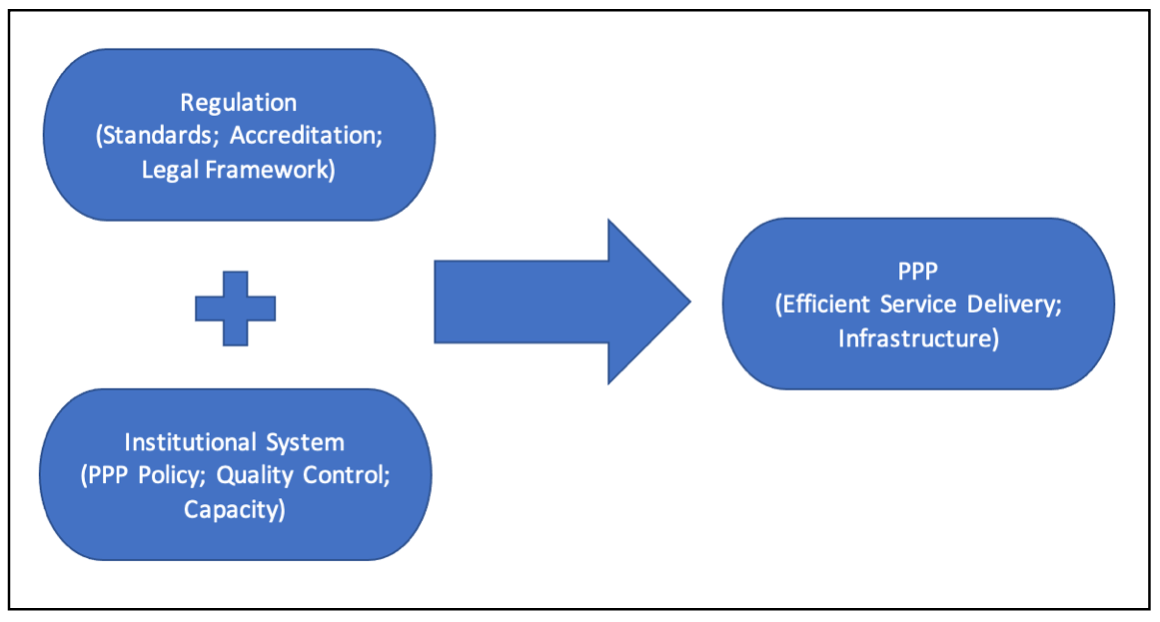
(Adapted from the book by A. Venkat Raman and J.W. Bjorkman: Public Private Partnership in Health Care in India: Lessons for Developing Countries, Routledge, London, 2009.)
It is widely recognised that daily consumption of iodised salt is the most cost-effective and efficient strategy to ensure adequate iodine intake across large populations. Salt, being a market commodity, is produced, packaged, and distributed by private players and sold in every corner of the country — from tribal hamlets to metropolitan supermarkets.
Over 95 per cent of salt production in India is handled by the private sector. In this context, the goal of sustainably eliminating IDD can only be achieved if the public and private sectors work in close coordination to ensure the availability, affordability, and quality of iodised salt.
The public sector bears the responsibility of safeguarding population health and nutrition, while the private sector possesses the technical knowledge and logistical infrastructure for salt production and distribution. Together, they form the two pillars upon which the success of India’s salt iodisation efforts rests.

As a result of this collaboration, India has achieved commendable progress towards the sustainable elimination of IDD. National surveys such as the National Family Health Survey (NFHS), the Comprehensive National Nutrition Survey (CNNS, 2016–18), and the India Iodine Survey (2018–19) affirm that cooperation from the salt industry has been a key driver of success.
Efforts to engage small- and medium-scale salt producers, with a focus on strengthening quality assurance protocols, have played a critical role in improving household coverage with adequately iodised salt.
The Way Forward
Despite the commendable progress, India is yet to reach the target of over 90 per cent coverage with adequately iodised salt — a crucial threshold for the sustainable elimination of IDDs.
As per data from the India Iodine Survey (2018–19), conducted jointly by AIIMS, Nutrition International, Indian Coalition for Control of Iodine Deficiency Disorders (ICCIDD), and Kantar (a leading global data, insights, and consulting company), only 76.3 per cent of the population consumes adequately iodised salt, while 92.4 per cent consume salt with some level of iodine.
With India’s estimated population at 1.39 billion (2021), 92.4 per cent coverage translates to roughly 1.28 billion individuals — equivalent to the combined population of 193 countries in the world!
Nevertheless, 23.7 per cent of the population still consumes either inadequately iodised salt (16.1 per cent) or non-iodised salt (7.6 per cent). This sizeable population remains at risk and needs urgent attention.

To close this gap and reach the ‘last mile’, the PPP model must be further strengthened and expanded. Greater investment in communication, quality monitoring, rural market access, and community engagement will be necessary to ensure universal coverage.
In conclusion, the harmonious partnership between public policy and private enterprise is the backbone of the USI programme’s success. The road ahead demands renewed commitment and innovation to ensure that no Indian child is denied the opportunity to grow, learn, and thrive — simply because of a preventable micronutrient deficiency.
(The author is President, Association for Indian Coalition for Control of Iodine Deficiency Disorders, an NGO based in New Delhi.)
Iodine Man of India
Retired as Professor and Head of the Department of Centre for Community Medicine at the All India Institute of Medical Sciences (AIIMS), New Delhi, Dr Chandrakant Sambhaji Pandav is popularly known as the “Iodine Man of India” for his path-breaking contribution to public health and nutrition.
Dr Pandav is currently a Member of the National Council on India Nutrition Challenges under the POSHAN Abhiyan, chaired by the Vice-Chairperson of NITI Aayog. He completed his MBBS and MD in Community Medicine from AIIMS, New Delhi, and is also an alumnus of the Department of Human Nutrition at the London School of Hygiene and Tropical Medicine, United Kingdom.
As the “Iodine Man of India,” he has been a relentless crusader in the global fight to eliminate Iodine Deficiency Disorders (IDD) — described by the WHO as the single most important preventable cause of mental disability worldwide. His pioneering research, sustained advocacy, and technical expertise have played a crucial role in the success of India’s National Iodine Deficiency Disorders Control Programme and in establishing mandatory Universal Salt Iodisation (USI), not only across India but in several countries worldwide.
Thanks to efforts spearheaded by Dr Pandav and his collaborators, iodised salt coverage in India surged from under 5 per cent in the 1980s to 93 per cent by 2018–2019. This single intervention is estimated to have saved 4 billion IQ points among Indian children since 1985 — an immense cognitive and economic gain for the country.
Dr Pandav’s pioneering contributions include the development of the concept of “Extra-Himalayan Fortification of Endemic Goitre”, which extended the scope of IDD prevention beyond traditional high-risk regions. He has also conducted comprehensive economic evaluations of the IDD control programme, providing definitive evidence of the cost-effectiveness and cost-benefit of iodisation interventions implemented at scale.
Dr Pandav is a founding member of the Iodine Global Network, recognised by the World Health Assembly as an International Non-Governmental Organisation (INGO). Since 1985, he has served as the Regional Coordinator for South Asia, contributing to global IDD control strategies.
He has served as a consultant to the WHO and UNICEF on iodine deficiency since 1983, working in over 60 countries across South Asia, the Western Pacific, the Middle East, and Africa. His work is widely acknowledged in the fields of IDD, micronutrient deficiencies, health systems research, health economics, policy formulation, programme evaluation, public–private partnerships, and human rights in health.
A prolific scholar, Dr Pandav has co-edited 14 books on health sciences and authored more than 600 research papers published in esteemed national and international journals.
Among his notable publications are “Elimination of Iodine Deficiency Disorders: Yes, It’s a Worthwhile Investment” and “SOS for a Billion,” which underscore both the urgency and feasibility of eliminating IDDs from public health systems worldwide.
Dr Pandav has received numerous prestigious national and international awards for his pioneering work. These include:
• The Dr M K Seshadri Prize and Gold Medal awarded by the Indian Council of Medical Research (ICMR) in 2000 for his outstanding contributions to the field of Community Medicine.
• Fellowship at the National Academy of Medical Sciences, New Delhi (2001).
• Fellowship of the Royal Institute of Public Health and Hygiene and the Society of Public Health, London.
• The Mother Teresa Memorial Award (2016) for his exemplary work in advancing USI.
In 2017, Dr Pandav was honoured with the WHO Public Health Champion Award for his long-standing, impactful contribution to public health, particularly in developing policy frameworks, strategies, and interventions that led to significant health improvements with equity.
In recognition of his exceptional and distinguished service in the field of medicine, Dr Pandav was conferred the prestigious Padma Shri Award in 2021, one of India’s highest civilian honours.
(As Conversation with Abhigyan K Tiwary)