Diabetes: Battling A Silent Killer
Recent reports indicate a significant rise in diabetes cases in India. Shockingly, one in every five diabetes patients worldwide is Indian. Double Helical delves into the complexities of the modern diabetes crisis, exploring innovative approaches for prevention and management…
By Amresh K Tiwary
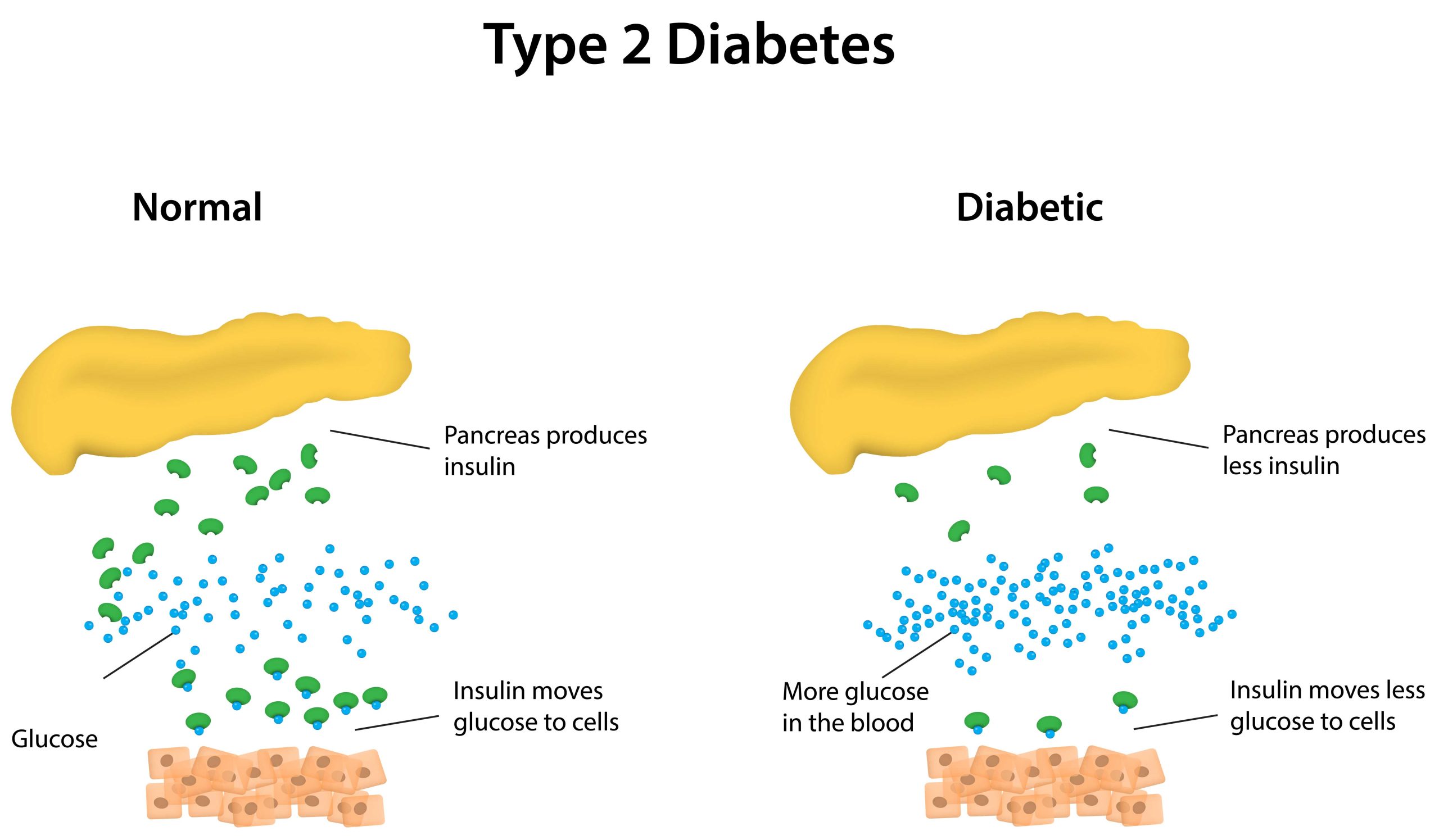
 Diabetes mellitus disrupts the body’s ability to produce or respond to insulin, a crucial hormone essential for converting sugar, starches, and other nutrients into energy needed for daily activities. Consequently, diabetes leads to abnormal carbohydrate metabolism and elevated blood glucose levels.
Diabetes mellitus disrupts the body’s ability to produce or respond to insulin, a crucial hormone essential for converting sugar, starches, and other nutrients into energy needed for daily activities. Consequently, diabetes leads to abnormal carbohydrate metabolism and elevated blood glucose levels.
Despite extensive research, the exact cause of diabetes remains elusive. However, it is evident that genetics and environmental factors such as obesity and sedentary lifestyles contribute significantly to its development.
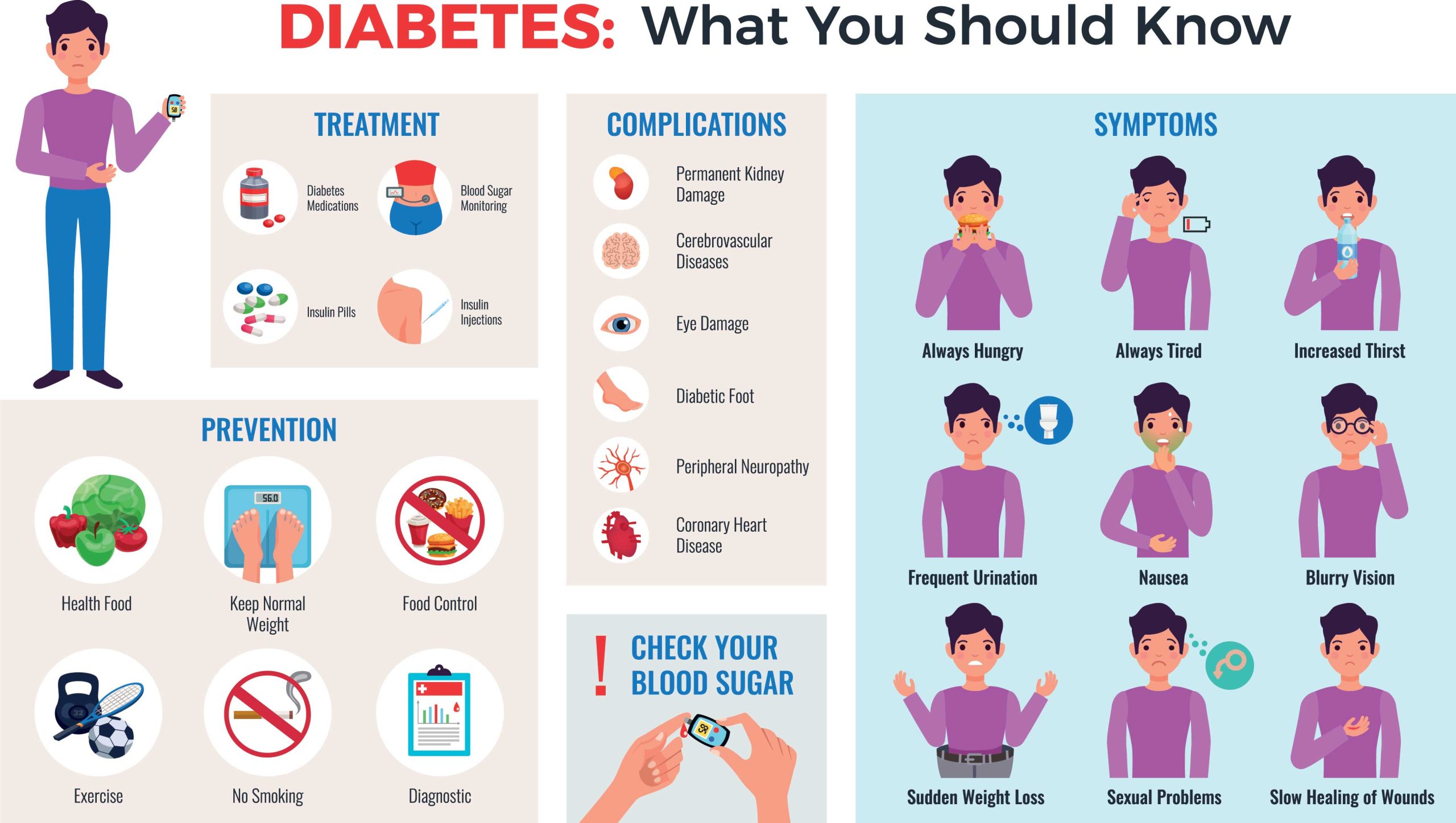
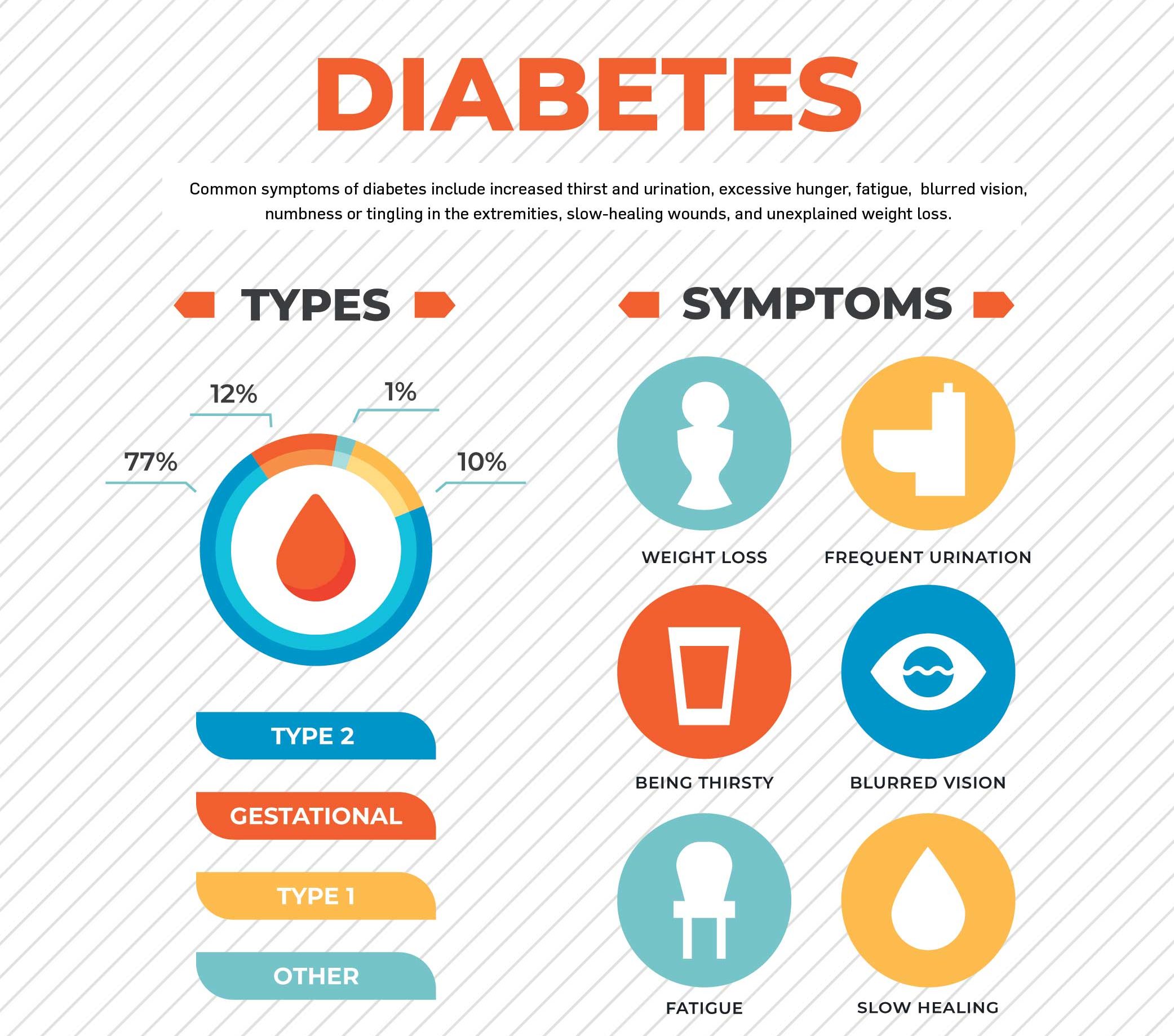
Common symptoms of diabetes include increased thirst and urination, excessive hunger, fatigue, blurred vision, numbness or tingling in the extremities, slow-healing wounds, and unexplained weight loss.
Understanding the root causes of diabetes empowers individuals to manage their symptoms effectively and adopt preventive measures. While some risk factors are modifiable, others are inherent to an individual’s genetic makeup. Early diagnosis of diabetes enables prompt intervention and facilitates the implementation of strategies for optimal self-care.
Diabetes encompasses a group of metabolic disorders characterised by hyperglycaemia, which arises from defects in insulin secretion, insulin action, or both. Prolonged hyperglycaemia is associated with chronic damage, dysfunction, and failure of various organs, particularly the kidneys, eyes, nerves, heart, and blood vessels.
The development of diabetes involves several pathogenic processes, ranging from autoimmune destruction of pancreatic beta cells leading to insulin deficiency, to abnormalities resulting in insulin resistance.
Types of Diabetes
Symptoms of type 1 diabetes can manifest rapidly, typically within weeks. Conversely, symptoms of type 2 diabetes often manifest gradually over several years, sometimes so subtly that they go unnoticed. Many individuals with type 2 diabetes may remain asymptomatic, with some only discovering their condition when complications such as blurred vision or cardiovascular issues arise.
Type 1 Diabetes: Type 1 diabetes results from the progressive destruction of beta cells, leading to severe insulin deficiency. While symptoms may appear suddenly, the underlying pathological changes occur over an extended period. The destruction of beta cells is believed to be an autoimmune process triggered by various environmental factors acting on a genetically susceptible individual.
Type 2 Diabetes: Type 2 diabetes, the most prevalent form of diabetes, is influenced by various factors, including lifestyle choices and genetic predisposition. Individuals who are physically inactive and overweight or obese are at a higher risk of developing type 2 diabetes. Excess weight can lead to insulin resistance, a common occurrence in type 2 diabetes.
Type 2 diabetes typically initiates with insulin resistance, a condition where muscle, liver, and fat cells fail to efficiently utilise insulin. Consequently, the body requires more insulin to facilitate glucose entry into cells. Initially, the pancreas compensates by producing extra insulin to meet this heightened demand. However, over time, the pancreas becomes unable to maintain sufficient insulin production, resulting in elevated blood glucose levels.
 The exact aetiology of type 2 diabetes remains unclear. Nonetheless, the primary underlying defects involve reduced insulin sensitivity and impaired beta-cell function. These defects set off a cascade of events leading to widespread metabolic imbalances and clinical manifestations. Type 2 diabetes often manifests gradually and progresses slowly.
The exact aetiology of type 2 diabetes remains unclear. Nonetheless, the primary underlying defects involve reduced insulin sensitivity and impaired beta-cell function. These defects set off a cascade of events leading to widespread metabolic imbalances and clinical manifestations. Type 2 diabetes often manifests gradually and progresses slowly.
In addition to type 1 and type 2 diabetes, there is a third type known as “1.5” type diabetes, or Latent Autoimmune Diabetes of Adulthood (LADA). LADA presents as a latent autoimmune disease with a slower onset compared to type 1 diabetes typically diagnosed in juveniles.
According to Prof (Dr) Anoop Misra, Executive Chairman of Fortis C-DOC Hospital for Diabetes and Allied Sciences in New Delhi, diabetes has been recognised since ancient times, with references found in Indian ancient treatises such as the Vedas, dating back over 4,500 years. The term “Diabetes” originates from the Greek word for ‘Siphon,’ reflecting the excessive urination observed in patients. The term “mellitus” is derived from the Greek word for ‘sweet,’ referring to the presence of sugar in the urine.
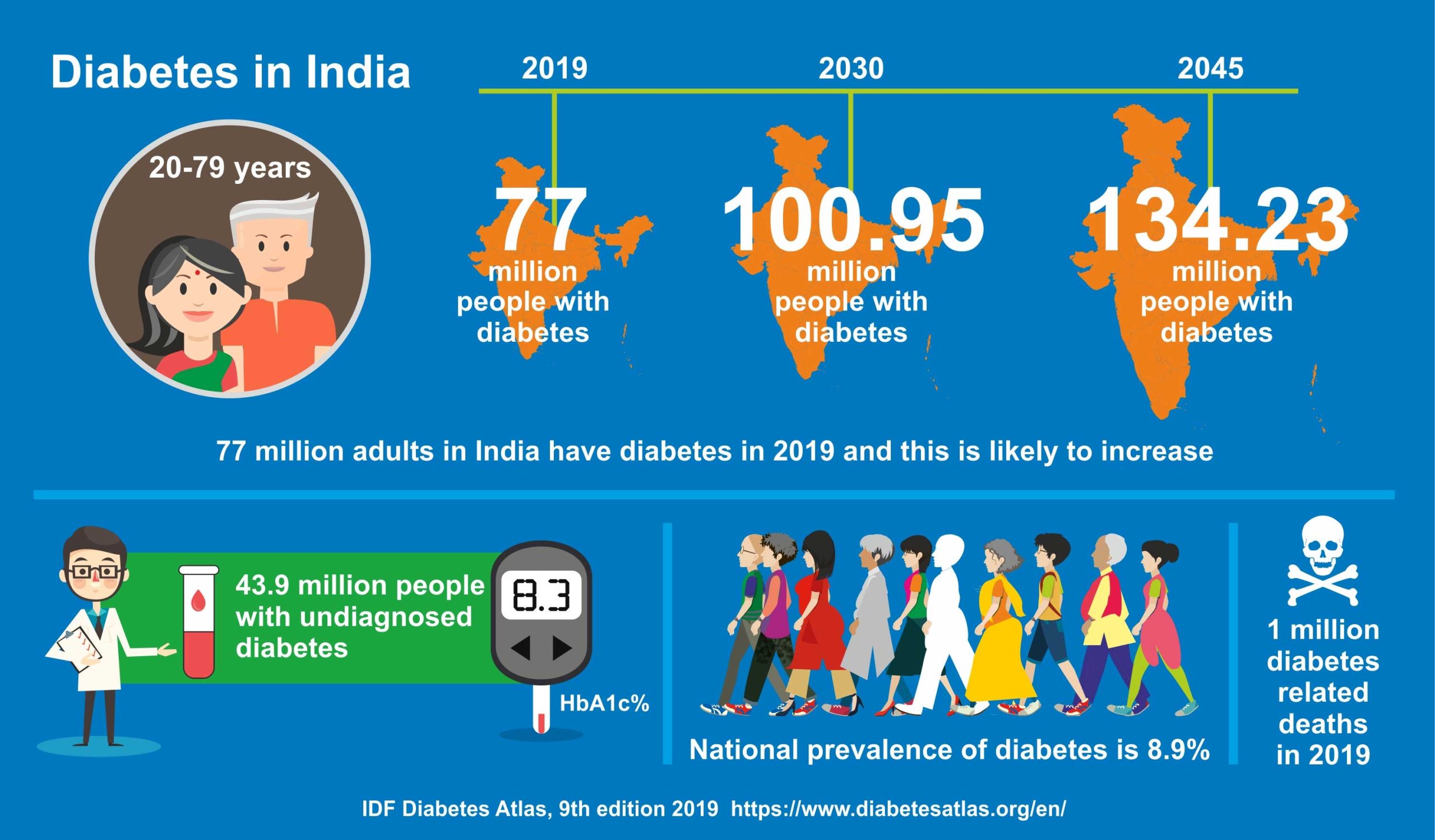
In India, more than 65 million people suffer from diabetes, and nearly 8 percent of the population above 18 years old is affected. This number is projected to increase to 100 million by the year 2030, making India second only to China in diabetes prevalence. Shockingly, one in every five diabetes patients worldwide is Indian. A study revealed that 37 percent of Delhi’s population suffers from diabetes or pre-diabetes. Indians have a genetic predisposition to diabetes, with nearly 75 percent of patients with type 2 diabetes having a family history of the disease.
Approximately 90 percent of type 2 diabetes patients in India are either overweight or obese, a trend that is on the rise. More than 60 percent of women living in urban areas of India are overweight or obese, putting them at an equal or sometimes higher risk for developing pre-diabetes, diabetes, and related complications compared to men. Alarmingly, an estimated one-third of school children in India are overweight or obese, with rates as high as 40-50 percent in major metropolitan cities.
Diabetes-related complications are more prevalent among Indians compared to other populations. Roughly one-fifth of diabetes patients develop retinal disorders leading to vision loss, while more than 50 percent suffer from diabetic neuropathy, resulting in sensory loss, non-healing foot ulcers, and impotence among men. India leads in the highest number of leg amputations due to diabetic foot issues globally. Additionally, 20-30 percent of patients with diabetic neuropathy require dialysis or kidney transplant for survival, as diabetes and hypertension are the leading causes of kidney failure in India. Silent heart attacks are also more common among diabetic individuals, and heart disease in diabetic patients tends to be more complex and carries a higher mortality rate.
Similarly, strokes are also common among diabetic patients. In India, the highest number of deaths occurs due to diabetes-related heart disease, surpassing the combined mortality rates of HIV/AIDS, malaria, and tuberculosis. Shockingly, every ten seconds, one person in India dies from a diabetes-related cause. The net losses in India’s national income from diabetes and cardiovascular diseases amounted to $336.6 billion between 2005 and 2015.
Why are Indians More Prone to Diabetes?
Prof (Dr) Anoop Misra explains that Indians are more susceptible to ‘Syndrome X’—a clustering of increased abdominal girth, high blood pressure, high blood sugar, and deranged blood lipids—which are the first steps toward diabetes. Indians tend to have excess body fat from birth, with a higher propensity for clustered fat in their bodies, up to 1.5 times more than white individuals from birth onwards. Most Indian children are born small, underweight, with elevated blood pressure and adiposity, predisposing them to develop diabetes in adulthood.
Resistance to Insulin Action: A combination of genetic factors and excess body fat, particularly around the abdomen and liver, leads to an inherent tendency for insulin resistance. This results in insulin acting slowly and only partially effectively.
Fatty Liver (Non-Alcoholic Fatty Liver Disease): Liver fat accumulation, unrelated to alcohol consumption, is common among Indians. Excessive fat deposition in the liver leads to sluggish metabolism and overproduction of sugar, particularly during night-time. Such fatty liver conditions may progress to dysfunction, cirrhosis, and even cancer.
Fatty Pancreas (Fat Accumulation in Pancreas):
Studies indicate that even individuals who are not overweight may experience fat accumulation in the pancreas, potentially leading to dysfunction of insulin-producing cells.
Sudden Transition to Modern Lifestyles: The shift towards a more modern lifestyle is exacerbating the diabetes problem among Indians. Many people now prefer ready-to-eat foods and lead sedentary lives, departing from the traditional frugal Indian lifestyle. These habits significantly increase the risk of diabetes.
Genetic Factors: Indians possess genes that predispose them more to diabetes compared to other ethnic groups. Genetic tendencies may incline individuals to accumulate excess body and abdominal fat, as well as have larger fat cells, which impede insulin action. For instance, experts have identified the ‘Myostatin’ gene, which may contribute to excess fat and low muscle mass in Indians. Various other genes, when combined with poor diet or physical inactivity, may lead to diabetes.
Treatment of Diabetes
Until 1990, treatment options for diabetes were limited to sulfonylureas (such as glyburide and glipizide) and biguanides (metformin) in addition to insulin. Sulfonylureas were once associated with heart problems, leading to the increased popularity of metformin during that period.
In recent decades, gliptines (DPP4 inhibitors) have gained prominence in the treatment of diabetes. However, it remains unclear whether these drugs replace Metformin or Sulfonylureas. Metformin, widely prescribed for treating type 2 diabetes, is often the initial medication recommended for patients. It works by lowering blood glucose levels through reducing the liver’s glucose production and increasing insulin sensitivity.

Sulfonylureas, their association with cardiovascular disease, and the influential Framingham study of 1980 ushered in a new era in diabetes management, known as cardiovascular metabolic diabetes.
Diabetes often leads to muscle wasting and weakness. While insulin has been a primary focus in type 1 diabetes treatment, it is perplexing that in type 2 diabetes, where 70 to 80 percent of patients have normal to high insulin levels, insulin injections are still administered. This remains a significant mystery.
Humulin (Recombinant DNA insulin), a synthetic insulin used to control high blood sugar in adults, effectively reduces elevated blood glucose levels in diabetic patients. Human insulin was anticipated to revolutionise diabetes treatment. Animal studies have demonstrated insulin’s potential to prevent cardiovascular changes, yet it remains puzzling why diabetics continue to experience cardiovascular disease.
According to Prof (Dr) Ramesh K Goyal, former Vice Chancellor of Delhi Pharmaceutical Sciences & Research University, diabetes is a prevalent issue among older adults. Approximately 20% of individuals over 65 years old have diabetes mellitus, with nearly half of them remaining undiagnosed. Unlike younger individuals with type 2 diabetes, obesity is less common among older diabetes patients.
Despite this, there are numerous misconceptions regarding the potential consequences of uncontrolled hyperglycaemia. In nursing homes, being underweight is as prevalent as being overweight. Therefore, nutritional management should focus on weight gain for underweight elderly patients as much as on weight loss for obese patients.
In addition to dietary adjustments and exercise, pharmacological therapy is often necessary to optimise blood glucose control. Target blood glucose ranges should be tailored to individual patients. For frail patients, fasting plasma glucose levels should range from 100 to 140 mg/dl, with postprandial values below 200 mg/dl.
The discovery of various classes of oral anti-diabetic agents has improved the prospects of achieving better control of hyperglycaemia with reduced risk of severe adverse events. Some of these agents, such as acarbose, miglitol, metformin, and troglitazone, do not induce hypoglycaemia when used as monotherapy, making them safer options. Metformin, in particular, appears to be especially beneficial for obese insulin-resistant patients. However, the available data on the safety and efficacy of troglitazone in the elderly is insufficient. Combining two or three oral anti-diabetic agents to delay the need for insulin therapy is now possible, although the long-term effects of this approach remain unknown, and concerns regarding the cost of polypharmacy persist.
The Ayurvedic View
Dr Tanuja Nesari, Director of the All India Institute of Ayurveda (AIIA) in New Delhi, explains that in Ayurveda, diabetes is known as Madhumeha (Madhu meaning ‘honey’ and Meha meaning ‘urine’). Madhumeha is categorised as Vataj Meha, a problem caused by the aggravation of Vata. Vata symbolises wind and dryness, and the characteristic deterioration of the body indicates Vata impairment. This type of disease leads to the maximum deterioration of dhatus (body tissues), affecting all vital organs.
The other primary cause of diabetes, according to Ayurveda, is impaired digestion. This impairment leads to the accumulation of specific digestive impurities known as ama, which accumulate in pancreatic cells and impair insulin production.
In Ayurveda, it’s believed that sugar levels can be managed with proper medication and a strict diet and lifestyle plan. Diabetes, being a chronic metabolic disorder resulting from insufficient insulin production or ineffective insulin use, can only be treated by rejuvenating the entire body.
 Daily Routine for a Diabetic
Daily Routine for a Diabetic
Wake-Up Time: Rise by 6 am in the morning, allowing ample time for exercise. Start the day with a glass of lukewarm water mixed with two teaspoons of fresh lemon juice.
Exercise: Regular physical activity is crucial for diabetic patients. Morning walks are highly recommended, and activities like yoga and meditation can help reduce stress and enhance mental clarity. If health permits, consider exercises such as jogging, swimming, or cycling.
Breakfast: For breakfast, have two slices of wholemeal bread with butter and fresh, warm milk. Seasonal fresh fruits can be consumed occasionally, with or without milk.
At Work: As an office-goer, ensure you have filling snacks on hand at all times, as it’s advised for diabetics not to let their stomachs remain empty. Instead of opting for cheese, chips, or crackers, choose a handful of nuts or seeds for variety. Sunflower seeds, pumpkin seeds, almonds, cashews, and walnuts are excellent choices.
Lunch: For lunch, prioritise steamed or lightly cooked green vegetables such as cauliflower, cabbage, tomatoes, spinach, turnip, asparagus, and mushrooms. Vegetable soup or boiled vegetables are also good options. Include two or three whole wheat bread (chapatis), sprouts, salad, boiled rice, lentils (daal), etc., according to your appetite. Finish your meal with a glass of buttermilk (salty lassi), which can be enhanced with roasted cumin seeds, black salt, grated ginger, and green coriander leaves.
Daytime Sleep: If you’re not working, avoid daytime sleep as it can increase Kledaka Kapha, a sub-dosha of Kapha that governs the protective mucous lining of the digestive system. Elevated levels of Kledaka Kapha can impair digestion, posing additional problems for diabetes patients.
Evening Snacks: Enjoy a glass of fresh fruit or vegetable juice for your evening snack. Alternatively, consider having Ayurvedic tea with roasted chickpeas.
Dinner: Keep your dinner light and avoid having too many items. Opt for boiled vegetables, sprouts, cottage cheese (paneer), or a bowl of salad made from fresh raw seasonal vegetables. Also, ensure you eat at least two hours before going to bed.
Bedtime: Retire before 10 pm and have a glass of fresh boiled warm milk before heading to bed.
Ayurvedic treatment for diabetes aims to rejuvenate the body to balance sugar levels and promote positive changes in the patient’s life. Ayurvedic medicines target the root cause of the disease, strengthen the patient’s immunity, improve digestion, and promote overall health. Alongside medication, dietary and lifestyle changes are recommended to rejuvenate the body’s cells and tissues, enabling proper insulin production.
Final Thoughts
Diabetes has evolved into a major public health concern, imposing a substantial burden on both society and the economy. From understanding its genetic underpinnings to addressing societal determinants, the battle against diabetes requires a multifaceted approach. With proactive prevention strategies, innovative treatments, and heightened awareness, we can strive to stem the tide of this global epidemic and safeguard the health and well-being of generations to come.

