A Deadly Triad
 Air pollutants and temperature fluctuations can exacerbate the adverse effects of pollens, leading to allergic disorders and increased susceptibility to viral infections. Addressing these detrimental interactions necessitates interdisciplinary approaches, large-scale interventions, and the integration of ancient indian wisdom into contemporary healthcare practices.
Air pollutants and temperature fluctuations can exacerbate the adverse effects of pollens, leading to allergic disorders and increased susceptibility to viral infections. Addressing these detrimental interactions necessitates interdisciplinary approaches, large-scale interventions, and the integration of ancient indian wisdom into contemporary healthcare practices.
By Dr Amitav Banerjee
During the last few decades, allergies and respiratory illnesses such as allergic rhinitis, bronchitis, and asthma have shown a rising trend globally, affecting people of all ages, from children to the elderly. While pollen allergies are seasonal and coincide with changing weather patterns, the increasing air pollution resulting from industrial and vehicular emissions exacerbates the environmental threats faced by individuals. Furthermore, temperature fluctuations may act synergistically to pose health risks, particularly aggravating cardiovascular conditions in the elderly.
Most studies have focused on examining the effects of pollution, pollen, and temperature fluctuations on human health separately. However, a proper ecological appraisal necessitates that these factors should not be considered in isolation due to their synergistic interaction, which impacts health.
Outdoor air pollutants, bio-aerosols, and chemicals originating from various sources may have adverse effects on people’s health when present above critical concentrations. These include carbon monoxide (CO), carbon dioxide (CO2), nitrogen oxides (NOx), particulate matter (PM), bio-aerosols such as pollens, fungal spores, bacteria, viruses, and chemical particles like sulfur dioxide (SO2) and ozone (O3).
In the Indian context, poor housing conditions associated with poverty introduce an additional factor of indoor air pollution, primarily due to the use of fossil fuels for cooking or heating, which poses the risk of fatal carbon monoxide (CO) poisoning. Furthermore, tobacco smoke exacerbates indoor air pollution if any household member is a smoker.
In addition to the aforementioned pollutants and chemicals, fluctuating temperatures also have a significant impact on human health, either in isolation or synergistically.
Air pollutants and temperature fluctuations can enhance the adverse effects of pollens through various mechanisms. Some pollutants can alter the physical, chemical, and biological properties of pollen grains. Different agents of air pollution may adhere to the surface of pollen grains. Pollutants such as particulate matter (PM), nitrogen dioxide (NO2), sulfur dioxide (SO2), and carbon monoxide (CO) can directly affect the physical and chemical properties of pollen grains, altering their surface characteristics or molecular structure and increasing their allergy-causing potential. Consequently, the number of allergens or sub-pollen particles containing allergens released into the environment may increase. These fragmented particles, often smaller than 3 microns, can bypass the mucociliary defense mechanism of the upper respiratory tract and penetrate deeper into the lungs.

PM can serve as a carrier of allergens by binding with airborne pollen and simultaneously modifying their allergen load and composition. Gases such as nitrogen dioxide (NO2) and ozone (O3) can also alter the allergenic properties of pollens through nitration reactions, leading to a modulated immune response. Pollens can also act as carriers of lipids, further impacting the immune response to allergens. Moreover, many pollutants can interact with pollen, causing biological changes such as altered viability, germination rates, and fertility.
Environmental temperatures play a crucial role in shaping the commencement, duration, and severity of the pollen season, exhibiting regional variations. Changes in temperature and the increasing levels of greenhouse gases can impact the quantity of allergens in several ways, including promoting increased and faster plant growth, higher pollen generation, increased allergenicity of pollen, and earlier and prolonged plant seasons. Climatic factors such as rainfall, temperature, humidity, and wind movements can further influence the density of pollens in the atmosphere, subsequently affecting human health.
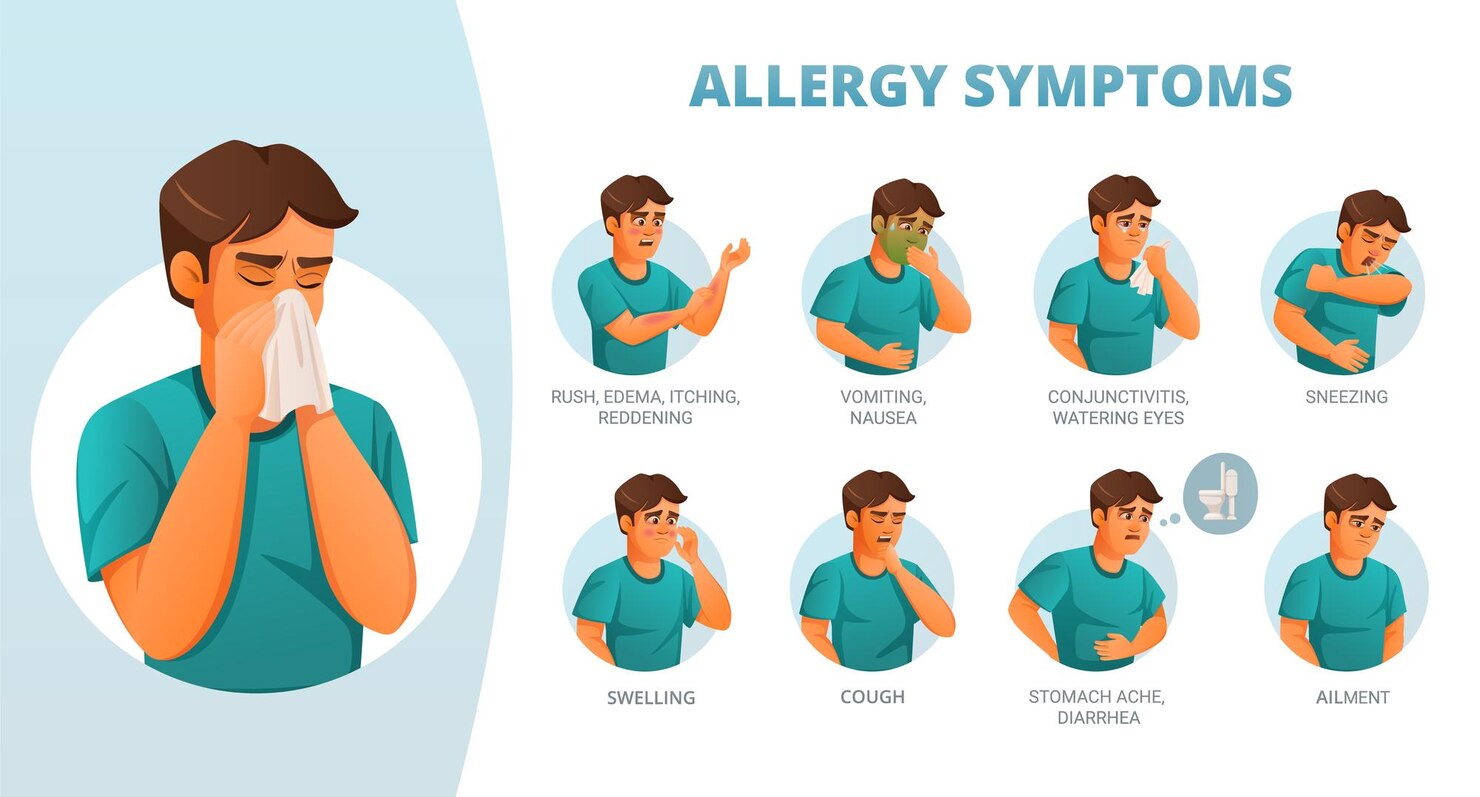
In such adverse environmental conditions, inhalation of allergens can lead to allergic disorders such as rhinitis, bronchitis, and asthma, while also influencing immune defenses and increasing vulnerability to viral infections. This disturbance of the immune system upon exposure to pollens is commonly observed in individuals with allergies but can also affect healthy individuals. For asthmatics, such environmental conditions can trigger bronchoconstriction and increased permeability of airway epithelium, exacerbating symptoms. Instances of allergic rhinitis tend to peak during such climatic conditions.

Skin conditions like allergic and atopic dermatitis are similarly exacerbated by seasonal factors and changing climates. Low humidity and cold temperatures can worsen atopic dermatitis, while low humidity can also dry the epithelial linings of the nose and throat, rendering them more susceptible to viral infections.
While the association between airborne pollens and cardiovascular diseases has not been extensively studied, there is a hypothesis suggesting that pollens could be a risk factor for heart attacks. This pathway may involve pollens activating mast cells, which subsequently lead to histamine release, potentially causing coronary artery spasm.
Studies indicate a combined effect of air pollution, pollens, and heat on population-level health outcomes, including an increase in respiratory morbidity and mortality. These effects are particularly relevant for individuals with existing heart and lung diseases. Temperature fluctuations, air pollution, and pollen exposure can trigger systemic and organ-specific inflammatory reactions, as well as cell damage, contributing to the exacerbation of these conditions.
Currently, there are significant research gaps in understanding the interaction between changing weather conditions, pollens, and air pollution, and their impact on public health. Research efforts should focus on studying their effects on various aspects such as birth outcomes and vulnerable populations, including children, pregnant mothers, the elderly, and individuals with a genetic predisposition to respiratory and cardiac diseases.
While there is considerable emphasis on the effects of heat, air pollution, and pollen on health, it’s essential to acknowledge that other environmental factors can also impact health. These factors may include occupational exposures, different types of air pollution mixtures, as well as airborne bacteria, viruses, molds, and fungi. In the real world, individuals are exposed to a complex combination of risk factors that may be poorly defined or understood, posing challenges for research. Furthermore, most diseases, especially non-communicable conditions, have multiple risk factors, such as genetic predisposition, unhealthy lifestyles, stress, and poor sleep quality. Future research into the causation of non-communicable diseases should consider environmental factors as effect modifiers or contributors to the causal pathway.
Additionally, factors like “immunity debt” and the “hygiene hypothesis” in the post-COVID period warrant further investigation.
The epidemiological triad model of disease causation comprises three factors: the agent, the environment, and the host. While discussing different agent factors such as air pollutants, pollens, and environmental conditions, it’s crucial to also consider host factors that contribute to people’s health. Understanding the interplay between these factors can provide valuable insights into disease prevention and management strategies.
In recent months, following the onset of winter and the post-pandemic period, there has been an uptick in childhood pneumonias, initially observed in China and later reported in countries across the Western hemisphere. These infections have been attributed to common respiratory viruses and pathogens. Notably, the outbreak coincided with China entering its first winter season since lifting its strict COVID-19 restrictions last December.
The organisms responsible for the outbreak in China are known pathogens, and no new virus or bacterium has been isolated. Maria Van Kerkhove, acting director of the WHO’s epidemic wing, suggested that the increase is likely due to children coming into contact with common viruses and bacteria from which they were somewhat protected during the COVID-19 restrictions.
Children typically experience repeated infections as they grow, which stimulate their immune system and contribute to the development of robust natural immunity. However, during the pandemic years, many children were deprived of this opportunity due to physical distancing and other non-pharmacological interventions (NPIs). This phenomenon has been termed the “immunity debt” or “immunity gap,” representing a short-term consequence of the “hygiene hypothesis.”
Professor François Balloux, an expert in computational biology at University College London, has squarely blamed China’s strict lockdown measures for the mystery pneumonia currently sweeping across the country. He suggests that China is experiencing waves of respiratory infections as it lifts its lockdown restrictions, particularly during its first winter season post-lockdown. The prolonged movement restrictions drastically reduced the circulation of respiratory pathogens, resulting in decreased natural immunity to common infections. Alongside usual viral infections such as Respiratory Syncytial Virus (RSV), influenza, and SARS-CoV-2, the surge is also driven by the bacterium Mycoplasma pneumonia.
Mycoplasma pneumonia infections occur throughout the year but peak every winter, with epidemics cyclically occurring every 3-4 years. However, due to China’s implementation of a longer and harsher lockdown than any other country, it is experiencing the steepest “lockdown exit” wave.
The descriptive epidemiology, which focuses on the distribution of cases among different age groups, lends support to the “immunity debt” hypothesis. Children, as a result of NPIs during the pandemic, have had limited exposure to common respiratory pathogens circulating in the community. In contrast, adults likely retain immune memory from pre-pandemic exposures.
This short-term “immunity debt” may lead to an accumulation of “interest” in later years, potentially resulting in a rise in allergic diseases. The distribution patterns of allergic conditions indicate a notable increase in more affluent regions with better hygiene and sanitation. “The hygiene hypothesis” suggests that early-life infections play a crucial role in immune system maturation, protecting against autoimmune diseases and allergies later in life. The higher incidence of autoimmune and allergic diseases may be attributed to decreased exposure to infections due to improved sanitation and healthcare.
To address diseases stemming from environmental factors such as pollen and pollution, scientists from the Post Graduate Institute of Medical Education and Research propose large-scale population-level measures. These include developing pollen forecasting systems, training healthcare workers and the public to interpret and respond to pollen forecasts, utilizing protective equipment like shields, spectacles, and air filters, and ensuring compliance with allergy medications. Emphasizing community awareness regarding pollen allergy, its symptoms, and management strategies is crucial.
These recommendations stem from a study sponsored by the Department of Science and Technology, Government of India, and published in the International Journal of Hygiene and Environmental Health. The study highlights the importance of proactive measures to mitigate the impact of environmental factors on public health.
Prof Khaiwal, the lead author of the study, advocates for a multi-stakeholder approach, emphasizing the importance of the education sector in developing capacity for aerobiological research, creating pollen forecast systems, and providing training for healthcare professionals.
In light of the COVID-19 pandemic, a study published in the Journal of the American Medical Association (JAMA) titled, “Benefits and Safety of Nasal Saline Irrigation in a Pandemic – Washing COVID-19 Away,” underscores the effectiveness of hypertonic nasal saline in promoting mucociliary clearance and reducing viral burden through physical removal. The nasal lining plays a crucial role in the innate immune system, serving as a primary defense against inhaled viruses, bacteria, pollens, and particulate matter. Saline nasal rinsing effectively eliminates pollutants and pathogens trapped in the nasal mucus.
Ancient Ayurvedic texts mention “Jal-Neti” or saline irrigation of the nasal passages as an essential personal hygiene practice. This raises the question of whether the ancient practitioners of Ayurveda were ahead of their time in recognising its benefits. Could regular “Jal-Neti” practice help prevent or treat conditions such as otitis media, asthma, sinusitis, and allergies?
There is a pressing need to invest more in research within the AYUSH systems of medicine and toward the development of an integrated healthcare system. Rather than waiting for the West to discover and teach us, we should embrace and explore the wisdom of our ancient traditions. .
(The author, an eminent epidemiologist and Professor at a Medical College in Pune, recently ranked in Stanford University’s list of the world’s top 2% scientists. He is also the author of the book, “COVID-19 Pandemic: A Third Eye.”)

