Decoding Barrenness
A staggering 30 million couples in India face the silent struggle of conception. However, a ray of hope shines through advancements in assisted reproductive technologies, offering respite to those on the arduous journey to parenthood. It’s imperative for couples to confront infertility as a shared challenge, breaking free from gender stereotypes…
By Abhigyan/Abhinav
Today, infertility has become a serious health issue with profound socioeconomic and health implications for both individuals and society. According to reports, out of the 60–80 million couples suffering from infertility globally each year, approximately 15 to 20 million (25 per cent) are in India alone.
The World Health Organization (WHO) states that one in every four couples in developing countries is affected by infertility. The magnitude of this problem necessitates urgent action, especially given that a significant portion of infertility cases is preventable. Despite the crucial consequences of infertility, estimating its prevalence remains challenging.
Recent advances in assisted reproductive technologies (ART) have expanded possibilities for successful infertility treatment. Notable examples of these technologies include intracytoplasmic sperm injection, oocyte donation, and embryo cryopreservation.
 According to a study conducted in nine Indian cities with 2,562 participants, nearly 46 percent were found to be infertile. Results from a parallel survey among 100 infertility specialists revealed that almost 63 percent of infertile couples belonged to the child-bearing age group (31-40).
According to a study conducted in nine Indian cities with 2,562 participants, nearly 46 percent were found to be infertile. Results from a parallel survey among 100 infertility specialists revealed that almost 63 percent of infertile couples belonged to the child-bearing age group (31-40).
Sudha Prasad, Director of Matritava Advanced IVF & Training Centre in Vasant Vihar, New Delhi, highlights that as life accelerates in the fast lane, infertility—a silent monster—gradually infiltrates the lives of urban Indians, causing sleepless nights and challenges in having children, especially among younger couples. It is ironic that, from a time when family planning drives launched in the 70s were the government’s primary focus, the country has reached a point where young and modern India seems to be grappling with the ever-increasing problem of infertility.
As Sudha Prasad elaborates, a journey through the infertility roller-coaster seems inevitable for many couples who, soon after marriage, realize how challenging it can be to conceive in today’s world. With the crisis escalating at a rapid rate, almost 30 million couples in the country suffer from infertility, resulting in an incidence rate of 10 percent for infertile couples. The number of Indian couples resorting to artificial methods to conceive has significantly increased today.
However, preventing infertility is not an impossible task; all that is required is tenacity, consistency, and determination in our day-to-day activities. Before delving deeper into the problem, it is important to understand what infertility is and how one defines it.
Dr Sudha Prasad emphasises that every human being wishes to procreate, and historically, infertility has been considered a curse for those affected by it. Couples may face difficulty conceiving naturally due to various reasons. Infertility centres nowadays offer comprehensive infertility management and ART programs to patients. Various forms of treatments, such as Intrauterine Insemination (IUI), In Vitro Fertilisation (IVF), Third-Party Reproduction, and Intracytoplasmic Sperm Injection (ICSI), are popular these days.
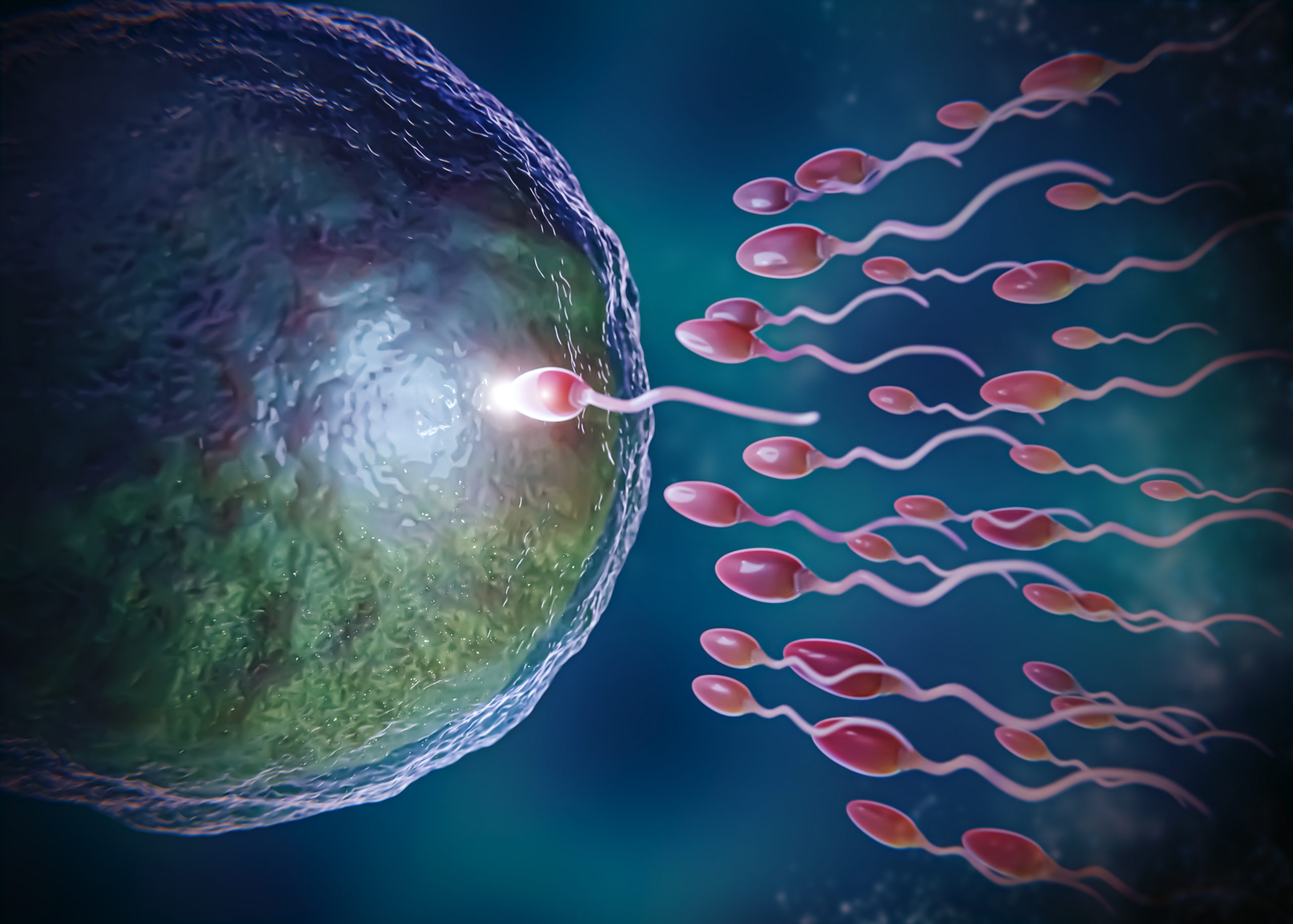
ICSI, pronounced “eeksee” or “icksy,” is an in vitro fertilisation procedure in which a single sperm is injected directly into an egg. The technique was developed by Gianpiero Palermo around 1991 in Brussels and has become the treatment of choice for men with weak sperm that cannot travel to the egg on their own.
 When can ICSI be performed?
When can ICSI be performed?
Men with obstruction in their passages can father a child by using their own sperms that have been extracted by a surgeon. ICSI can also be offered to patients of previous IVF failures due to failed fertilisation and patients with unexplained infertility. ICSI is different from conventional insemination since we clean away the follicle cells from around the eggs and an embryologist chooses the sperm to be injected. A small number of eggs do not tolerate the injection procedure and you can expect that about 5 per cent of eggs die as a direct result of ICSI. However, fertilisation rates, embryo quality and pregnancy rates are the same as for couples who do not have ICSI.
How is ICSI performed?
The process involves the injection of a single sperm within the ooplasm of the oocyte. Following the first ICSI birth in 1992, thousands of babies have been born around the world. Sperms for ICSI can be obtained from ejaculation, even when only few are present, or through surgical retrieval from epididymis or testis.
Microinjection is normally performed under a specialised microscope with the aid of a micromanipulator which allows small movements under high magnification. The scientist/embryologist sits on the ICSI station, looks either directly into the microscope or at a monitor that magnifies the image and then injects the egg by moving two manipulators that look and function like joysticks. He holds the oocyte with one hand and injects through the other.
ICSI (Intracytoplasmic Sperm Injection) can be performed in various situations, including:
Obstruction in Passages: Men with obstruction in their reproductive passages can use their own sperm, which has been extracted by a surgeon, to father a child through ICSI.
Previous IVF Failures: ICSI can be offered to patients who have experienced failed fertilisation in previous IVF attempts.
Unexplained Infertility: Patients with unexplained infertility, where the cause of fertility issues is not clear, may also be candidates for ICSI.
ICSI is distinct from conventional insemination methods. In ICSI, follicle cells surrounding the eggs are removed, and the embryologist selects a sperm for injection. Approximately 5 per cent of eggs may not tolerate the injection procedure, resulting in their death. However, the fertilisation rates, embryo quality, and pregnancy rates with ICSI are comparable to those without ICSI.
Procedure of ICSI
Injection Process: The procedure involves injecting a single sperm directly into the ooplasm (the cytoplasm of the egg).
Post-ICSI Births: Since the first ICSI birth in 1992, thousands of babies worldwide have been born through this procedure.
Sperm Source: Sperm for ICSI can be obtained from ejaculation, even in cases where only a few sperm are present, or through surgical retrieval from the epididymis or testis.
Microinjection Process: Microinjection is typically performed under a specialised microscope with the assistance of a micromanipulator, allowing small, precise movements under high magnification.
Embryologist’s Role: The scientist or embryologist, stationed at the ICSI station, either directly observes the microscope or views a monitor magnifying the image. They inject the egg by manipulating two joysticks, holding the oocyte with one hand and injecting through the other.
ICSI has proven to be a successful technique, offering hope to couples facing male factor infertility or other challenges in natural fertilisation.
 IVF Process
IVF Process
IVF (In Vitro Fertilisation) is a reproductive technology that enables mammals, including humans, to reproduce through a process that takes place outside the woman’s body. Here is an overview of the IVF process and the evaluation and preparation of couples:
Definition of Reproduction: Reproduction involves the fusion of male and female gametes, resulting in the exchange of genetic material and the formation of a new individual with a unique genotype.
Sexual Reproduction in Mammals: Mammals typically reproduce through sexual reproduction. However, advancements in technology now allow mammals to reproduce “asexually” through in vitro fertilisation.
IVF Technique: In IVF, the entire fertilisation process occurs outside a woman’s body. This involves the extraction of a woman’s eggs, fertilisation of the eggs in a laboratory setting with sperm, and the subsequent transfer of resulting embryos into the woman’s uterus through the cervix (embryo transfer). The embryo can then develop within the uterus.
Embryo Transfer: Typically, couples transfer two embryos, although more may be transferred in certain cases.
Indications for IVF: IVF is commonly used in cases where a woman has blocked, severely damaged, or absent fallopian tubes. It is a common form of Assisted Reproductive Technology (ART).
Evaluation and Preparation of a Couple: Proper evaluation of an infertile couple before undergoing IVF is crucial for the success of the procedure and the prevention of complications.
Fertility Workup: Any ART procedure, including IVF, should be preceded by a traditional fertility workup. At this stage, a decision is made on whether to proceed with ART, postpone for other treatment modalities, or refuse the procedure for the couple.
Thorough Testing: Once the decision to undergo ART, specifically IVF, is made, a thorough testing of the patient is undertaken to identify and correct any issues that may lead to IVF failure.
Consideration of Specific Procedures: At this stage, decisions are made on whether specific procedures such as egg, sperm, or embryo donation are required for the success of IVF.
Third-Party Reproduction
Third-party reproduction involves the utilisation of oocytes, sperm, embryos, or a uterus provided by a third person (donor) to assist a couple or a single individual (intended parents) in becoming parents.
According to current Indian guidelines on Assisted Reproductive Technology (ART) established by the Indian Council of Medical Research (ICMR), all donors, with the exception of surrogates, must remain anonymous to the commissioning couples. The guidelines further stipulate that the provision of various gametes and surrogates is not conducted by the IVF centre itself but by separate entities known as ART Banks. These banks are also responsible for handling all legal issues associated with third-party reproduction. Once the necessary requirements are met, the medical fitness of the donor or surrogate is assessed, and after completing the required formalities, the couple, along with their donor or surrogate, is enrolled in the third-party program.
Recurrent Pregnancy Loss (RPL) Programme
Experiencing repeated pregnancy losses can be emotionally devastating for both the patient and the treating doctor. RPL is defined as a situation where a woman has lost three or more pregnancies. Chronic infections such as genital tuberculosis may contribute to RPL. Additionally, impaired blood circulation within the pelvis, particularly the uterus, has been identified as a major cause of recurrent failures, whether during implantation or later stages of pregnancy.
In addressing RPL, a comprehensive approach is often required to identify the specific causes and factors contributing to repeated pregnancy losses. The understanding that impaired blood circulation can be a significant factor highlights the importance of thorough investigation and targeted interventions to improve the chances of a successful pregnancy for individuals facing recurrent pregnancy loss.
Doctors conduct tests to identify the causes of Recurrent Pregnancy Loss (RPL) and tailor treatment accordingly. If a genetic cause is identified, the patient and her husband are informed about the defect, and counselling is provided regarding future implications. Endocrine causes, such as Polycystic Ovary Syndrome (PCOS), may contribute to RPL and can be addressed with insulin-lowering medication. It is important to note that extensive testing is not typically recommended after a single pregnancy loss, as this may have occurred by chance, and there is no need for undue concern.
Male Infertility Programme
Throughout history, the responsibility for procreation has often been attributed to women. Research and advancements in medication and technology for infertility primarily focused on female-related issues. While these innovations improved success rates in female infertility, the male counterpart received less attention, partly because infertility was traditionally within the realm of gynaecologists. Moreover, in developing countries like India, there was reluctance among males to accept themselves as the potential cause of infertility in a couple.
However, the last century witnessed rapid advances in the management of male infertility, encompassing diagnostics and treatment. The WHO provided guidelines for proper semen examination, forming the basis for treatment recommendations. This shift marked a significant change, acknowledging and addressing male infertility issues, which had previously been overlooked. The denial among males about their potential role in infertility started to diminish, allowing for more comprehensive care and support for couples facing fertility challenges.
Contemporary male infertility programs go beyond standard testing procedures, such as semen analysis, to include specialized tests assessing the fertilizing potential and quality of sperm. One such test is the DNA fragmentation test, which evaluates the integrity of sperm DNA.
For patients diagnosed as azoospermic (no sperm in the ejaculate) on initial testing, testicular fine needle aspiration is typically performed. If this procedure also fails to yield sperm, doctors may proceed to a testicular biopsy. In the biopsy, the sample is examined for the presence of sperm. If sperm are identified, they can be frozen or cryopreserved until the wife is prepared for Intracytoplasmic Sperm Injection (ICSI) during In Vitro Fertilisation (IVF).For men with mild male factor infertility, Intrauterine Insemination (IUI) may be offered. However, for those with weak sperm, more advanced techniques like IVF or ICSI may be recommended. IMSI (Intracytoplasmic Morphologically Selected Sperm Injection) is a specialized sperm selection method used within ICSI. This technique involves using a microscope to view highly magnified and detailed images of sperm, allowing the embryologist to select the best sperm for injection into an egg.
These advancements in testing and treatment modalities within male infertility programs contribute to more precise diagnostics and tailored interventions, enhancing the chances of successful fertility outcomes for couples facing male factor infertility.
Infertility in Couples
By Dr Sowjanya Aggarwal

Infertility is characterized by the difficulty in conceiving or achieving pregnancy despite engaging in regular unprotected sexual intercourse for one consecutive year. The duration it takes for a couple to conceive can vary, ranging from days to months. Traditionally, infertility was often perceived as exclusively a ‘female problem,’ subjecting women to social ridicule.
Surprisingly, around 40 per cent of fertility issues in couples can be attributed to male subfertility. In addressing this, Intracytoplasmic Sperm Injection (ICSI) has emerged as a breakthrough treatment, becoming the preferred method in assisted reproduction for predominantly male-factor infertility.
Experts emphasize that assistance can be provided to both men and women based on the underlying cause of infertility. Infertility management entails comprehensive investigations to arrive at a logical diagnosis and subsequent targeted treatment. The outdated notion of solely blaming women for infertility has become obsolete. Research findings have unveiled that male factors contribute significantly to infertility.
Presently, research indicates that one in every five men within the age group of 18 to 25 experiences abnormal sperm count, a primary contributor to infertility. This awareness underscores the importance of considering both male and female factors in the diagnosis and treatment of infertility, fostering a more holistic and effective approach to assisted reproduction.
The widespread issue of infertility prompts the question of its underlying reasons. Irregular and low sperm count, compromised sperm delivery and motility (the ability to move efficiently through the female reproductive system for fertilisation), stand out as prominent causes of male infertility. Medical factors like obesity and lifestyle disorders, including diet imbalance, smoking, alcoholism, sedentary living, and mental stress, contribute to poor sperm count.
In women, conditions such as Polycystic Ovary Disease (PCOD), characterised by hormonal imbalances and lack of ovulation, along with a demanding lifestyle and job stress, can lead to conception problems. Primary Ovarian Insufficiency (POI), causing ovulation problems, occurs when ovaries cease normal function before the age of 40. Changing lifestyle patterns, demanding work schedules, and stressful environments also contribute to fertility issues.
Despite the challenges, there are preventive measures that individuals can adopt. General measures like maintaining a healthy weight, avoiding cigarettes and alcohol, managing stress, and having a nutritious diet are vital. However, specific factors impacting fertility are often overlooked.
High testicular temperature is increasingly recognized as a cause of male infertility. Prolonged use of mobile phones, associated with intense and prolonged radiation, can harm sperm production. Men are advised to wear loose underwear, avoid resting laptops on laps, and take breaks during prolonged sitting. Certain sports may pose risks to testicular health, and injuries should be promptly treated to prevent long-term consequences on fertility.
Declining libido among urban couples emerges as a significant cause, driven by hectic schedules, poor work-life balance, constant tension, and increased travel time. Stress, unhealthy eating habits, and medical conditions like diabetes contribute to poor sperm and egg quality. To address these issues, habits such as smoking, tobacco consumption, frequent drinking, unhealthy eating, and lack of exercise should be promptly addressed. Adopting these preventive measures is crucial in fostering reproductive health in both men and women.
It might come as a surprise that household products such as furniture polish, all-purpose cleaners, bug sprays, bathroom cleaners, and room deodorizers may contain chemicals that could reduce conception rates by up to 33 per cent. Opting for organic, non-toxic alternatives is a safer choice.
Additionally, prioritizing good sleep is crucial, as 80 per cent of ovulation occurs between midnight and 4 am. Interrupted sleep patterns can weaken immunity, disrupt reproductive hormone levels, and hinder ovulation.

