The Unique Epidemiology of Diabetes
The epidemiology of diabetes in India is unique. The determinants are both “nature” and “nurture,” against the background of malnutrition at both ends of the life course….
 By Dr Amitav Banerjee
By Dr Amitav Banerjee
According to a report, hundred million plus Indians have now diabetic, up 44% in 4 years while ICMR study says that the research brought out that while 11.4% of India’s population is diabetic, a larger proportion, 15.3% is pre-diabetic.
India has now more than 101 million people living with diabetes, compared to 70 million in 2019. Part of the increase may be due to better awareness among the people leading to increased detection. Another factor may be better care and longevity of diabetics who pass on the genotype to their progenies increasing the diabetogenic gene pool. Having said this, there are short term and long term challenges given the complex epidemiology of diabetes in our country.
The epidemiology of diabetes in India is unique. The determinants are both “nature” and “nurture,” against the background of malnutrition at both ends of the life course; under-nutrition in the uterus and early childhood, and over-nutrition in adult life. Adding to the diabetes burden are socioeconomic changes and market forces nudging the newly rich and burgeoning Indian middle class’s cravings for fast food, cola drinks, and drift towards a sedentary lifestyle.
The Intrauterine origins of metabolic syndrome and adult onset Diabetes Mellitus
Dr David Barker proposed the foetal origins of adult disease (FOAD), which became popularly known as the Barker’s hypothesis. This stipulates that events during the early developmental stages of life starting from intra-uterine period have a profound impact of developing diseases in adulthood. Low birth weight which can be taken as a surrogate measure of intra-uterine growth restriction can predispose individuals to insulin resistance in adult life, besides a host of other conditions including obesity and diseases of the cardiovascular system.
Barker, a British epidemiologist, put forth that inadequate nutrition in utero programs the foetus to have metabolic characteristics that can lead to future disease. He argued that individuals starved in utero are more likely to become obese during adulthood and suffer from conditions associated with it which includes Type 2 diabetes.
The Thrifty Gene Hypothesis – Muqaddar or Destiny.
The thrifty gene hypothesis attempts to explain the high prevalence of obesity, metabolic syndrome, diabetes mellitus and cardiovascular diseases in populations undergoing rapid economic growth. The thrifty gene hypothesis proposes that genetic features that promoted accumulation of fat around the waist (central obesity) helped individuals with such genotype to survive periods of deprivation such as great famines. Populations which have experienced such famines consist of higher proportion of individuals with the “thrifty gene” as according to Darwinian principles they are adapted to survive in harsh times compared to those without the thrifty gene. India has had its share of harsh famines in the past such as the Agra and Bihar famines in the nineteenth centuries and the Bengal famine in the twentieth century under British rule, to name a few. It follows that it would have a large proportion of individuals with this genetic programming.
Unfortunately, this “genetic programming” which helped individuals to survive during periods of famine, acts as a “bug” in times of calorie abundance. Populations which have faced deprivations in the past and are presently experiencing rapid economic growth with an expanding middle class tend to consume excess fast foods and reduce their physical activity. High proportion thrifty genes carried over from a previous era of famine and deprivations leads to a high prevalence of metabolic syndrome which is a combination of central obesity, an increased risk of insulin resistance, diabetes mellitus, and vascular and neurological complications such as coronary events and stroke.
While providing a neat explanation for the lay audience, the evidence to support the thrifty gene syndrome is still a work in progress.
Life Course Strategy to change the destiny
As you might have seen the superhit movie “ Muquaddar Ka Sikandae”, “Muqaddar” means destiny and “Sikandar” stands for a conqueror. A large proportion of Indians carry the genetic handicap either due to past deprivations such as famines or an unacceptable level of intrauterine and early childhood under-nutrition, predisposing them to develop metabolic syndrome. This is their destiny or handicap. To conquer this, a life course approach is indicated to control the burden of diabetes and metabolic syndrome in the long run.
The latest National Family Health Survey (NFHS-5), 2019-21, revealed 36% of under-five children in India are stunted (short for age), 19% are wasted (thin for their height), and 32% are underweight (thin for their age) all signs of early child malnutrition. These children mostly born to mothers with low level of schooling and in the lowest quintile of wealth may have faced intrauterine growth retardation too. Almost 20% of newborns in India have low birth weight which indicates intrauterine growth restriction.
These children who face foetal and early child nutritional deprivation will be at high risk for developing diabetes and metabolic syndrome in adulthood. To prevent future cohorts of under-nourished children contributing to the next generation of adult diabetics we urgently need to address our problems of maternal and child under-nutrition.
What about those who could not escape the destiny of early life malnutrition? They can also change their destiny by resisting lifestyles which predispose them to the risk, “the nurture” aspect. While genetic programming or early life deprivations might have predisposed large proportion of individuals in poor countries to risk of metabolic syndrome, lifestyle can play an important role in keeping metabolic syndrome and related conditions under control. Behaviour and environment can influence the genotype not expressing itself so that optimum health is achieved.
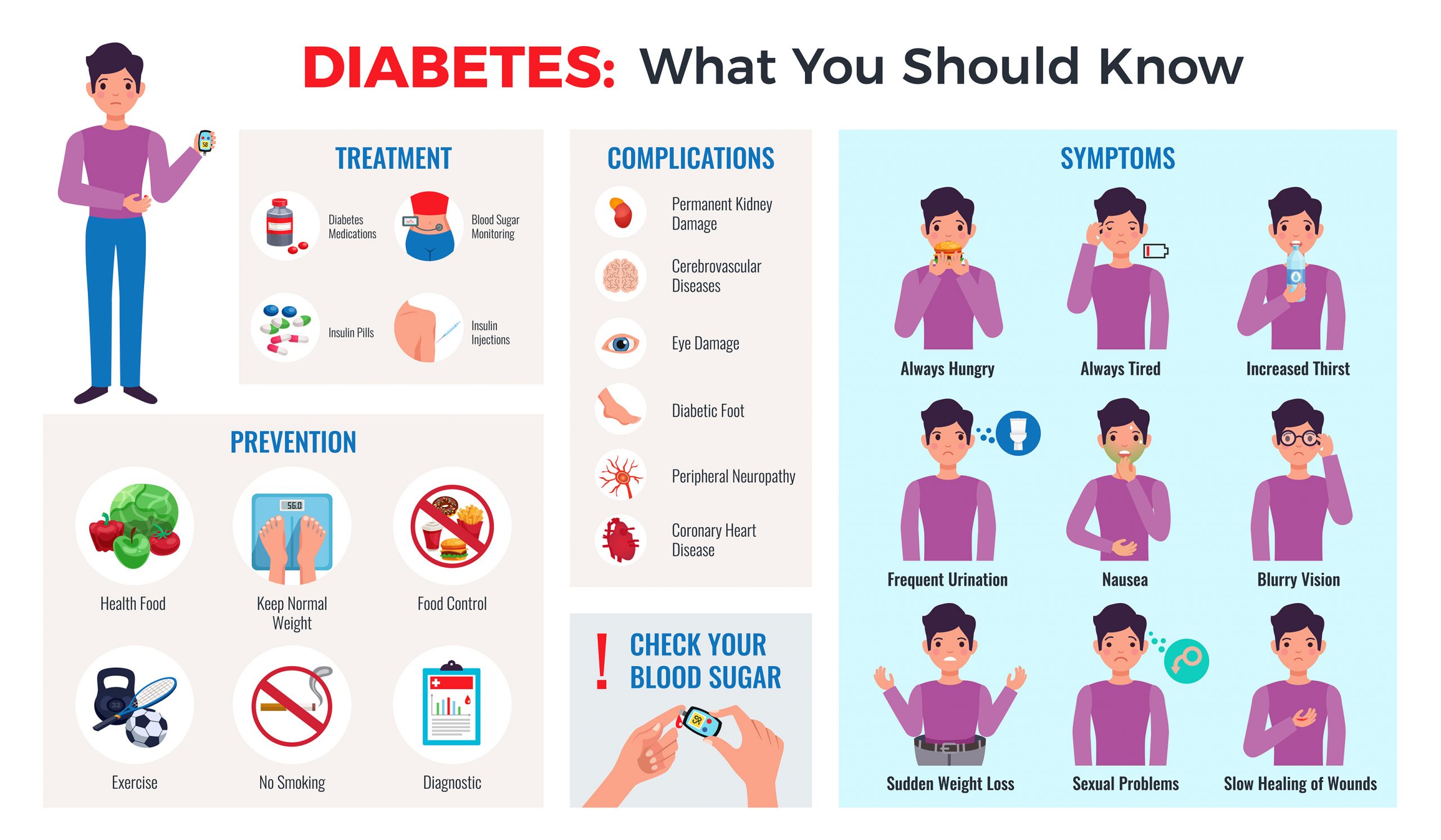
Diet and exercise can result in good health in spite of a genetic handicap which is not set in stone. Many early diabetics and pre-diabetics can achieve optimum health by lifestyle modifications which include a healthy diet, physical activity, avoidance of sugar, tobacco and alcohol and maintaining an ideal body weight. Some diabetics can reduce their anti-diabetic medications or go off them altogether if they can discipline themselves to maintain this lifestyle. Of course any reduction in medication or doing away with them altogether should be undertaken under expert supervision of their physician. Since vast swathes of our population are at risk the population approach to prevention by promoting better maternal and early child nutrition and physical activity and healthy diets throughout the life course will have long lasting impact on control of diabetes in the population.
Market forces and wrong role models are obstacles to lifestyle or population approach.
The major challenge in this approach is the strong influence of market forces targeting the neo-rich. Popular sportspersons, who are role models, advertising for sugary soft drinks and colas are an all too common sight. There are few exceptions such as Pullela Gopichand, the Indian badminton star who refused to advertise a soft drink brand at the peak of his career.
Secondary Prevention: taking care of the diabetics: crucial role of primary care.
Primary care should be pivotal in diabetes management. We have limited number of endocrinologists. Primary care providers will be the sheet anchor for managing diabetes in the community. This is challenging due to increasing complexity of anti-diabetic medications and monitoring of blood sugar levels and the need to avoid hypo and hyperglycemia in addition to counselling on lifestyle modifications.
Patient’s participation in management of diabetes
In a chronic disease like diabetes, the patient has an equally important role, if not more, in management. Self monitoring of blood glucose using a “fingerstick” method using a glucose meter and HbA1c which is a simple blood test that measures the average blood sugar level over the past three months are frequently used to monitor patients with diabetes. Self glucose monitoring can be easily learned by patients.
Recent advances in diabetes management include the continuous glucose monitoring (CGM) technology which can improve overall glycemic control while minimizing hypoglycaemia. However, its use is not widespread yet.
Patients should also be educated in care of the feet as diabetic foot is a common complication. Smoking cessation and abstinence or moderation in alcohol consumption, regular screening of eyes for cataract and retinopathy, kidney function tests and tests for cardiac function are done periodically to identify any target organ involvement.
Exercise, diet and anti diabetic medications under supervision and periodic review by the physician are important measures for management of this chronic condition.
(The author is Professor, DY Patil Medical College. Pune and an Academic Editor at PLOS ONE)

