Waging War On Black Fever
Dr C P Thakur has revolutionised the treatment of Kala-azar (KA) or Black Fever, a chronic and potentially fatal parasitic disease. As India has missed the 2017 deadline for KA’s elimination, his extensive research provides key insights into evolving situation of KA in the country as well as its cure and prevention aspects
By Amresh Kumar Tiwary
 Dr Chandreshwar Prasad Thakur, famously known as C P Thakur (born 3rd September, 1931), is a leading politician as well as a renowned doctor. Over the years, his clinic at Frazer Road, Patna has offered a large number of patients excellent treatment for various health issues. He is known to take care of patients with an immense amount of sensitivity for them and their families.
Dr Chandreshwar Prasad Thakur, famously known as C P Thakur (born 3rd September, 1931), is a leading politician as well as a renowned doctor. Over the years, his clinic at Frazer Road, Patna has offered a large number of patients excellent treatment for various health issues. He is known to take care of patients with an immense amount of sensitivity for them and their families.
Dr Thakur is recognized as an international authority in the treatment of Kala-azar (KA). and post Kala-azar dermal leishmaniasis. He was conferred the coveted Life time Achievement Award by the World Health Organization (WHO) for his extensive research in the field of KA, thus becoming the first Indian medical scientist to get this prestigious award from the WHO.
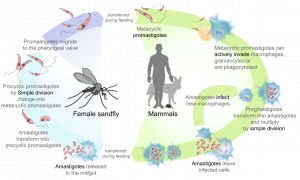
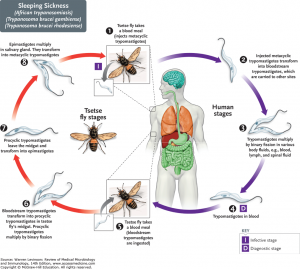
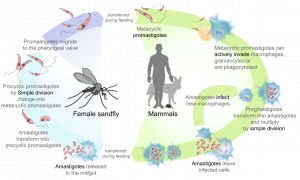
Kala-azar (visceral leishmaniasis, VL) is a major public health problem in many states of India including Bihar, affecting the poor sections of the society. KA is a slow progressing indigenous disease caused by a protozoan parasite of the genus Leishmania. The parasite primarily infects the reticulo-endothelial system and may be found in abundance in bone marrow, spleen and liver.
The word kala-azar consists of Kala (in Hindi means “Black”) and “azar” (in Hindi means Fever). Fever associated with dark complexion “Black Sickness” is a form of the disease leishmaniasis marked by emaciation, anaemia, fever, and enlargement of the liver and spleen. If left untreated for over two years, it can prove fatal. A person suffering from KA dies after catching another infection such as tuberculosis or severe anaemia.
 The disease has been targeted for elimination. In fact, the National Health Policy, 2002 had set the goal of KA elimination by the year 2010 which was further revised to 2017. India has missed the 2017 deadline that the Government of India had announced for elimination of KA in last year’s Budget. In fact, endemic blocks have increased from 61 to 68 in 17 districts of Bihar and Jharkhand.
The disease has been targeted for elimination. In fact, the National Health Policy, 2002 had set the goal of KA elimination by the year 2010 which was further revised to 2017. India has missed the 2017 deadline that the Government of India had announced for elimination of KA in last year’s Budget. In fact, endemic blocks have increased from 61 to 68 in 17 districts of Bihar and Jharkhand.
The matter was taken up at a meeting of the health ministry, recently. Officials told health secretary Preeti Sudan that a request to the Ministry of Rural Development for expediting construction of concrete houses, pending since 2001-02, was the primary reason behind the failure to control the disease.
Elimination is defined as reducing the annual incidence to less than 1 case per 10,000 people at the sub-district level.
Further, a little-known skin condition called Post Kala Azar Dermal Leishmaniasis (PKDL) — a red flag for transmission of Kala Azar has been growing steadily over the past few years. In recent times endemic blocks have increased from 61 to 68 in 17 districts of Bihar and Jharkhand.
 According to Dr C P Thakur, KA may be eliminated if we take up elimination programme with renewed vigour, effective drugs, better insecticides and strict supervision. Given the focal nature of the disease, availability of effective interventions including newer drugs and diagnostics, absence of animal reservoir in the Indian subcontinent, it should be possible to eliminate KA from India within the time frame. This would, however, require close monitoring and evaluation of Programme activities, by reaching out to interested experts/individuals and institutions for technical support.
According to Dr C P Thakur, KA may be eliminated if we take up elimination programme with renewed vigour, effective drugs, better insecticides and strict supervision. Given the focal nature of the disease, availability of effective interventions including newer drugs and diagnostics, absence of animal reservoir in the Indian subcontinent, it should be possible to eliminate KA from India within the time frame. This would, however, require close monitoring and evaluation of Programme activities, by reaching out to interested experts/individuals and institutions for technical support.
At present, all programmatic activities are being implemented through the National Vector Borne Disease Control Programme. It is now opportune time to review the situation and assess the current challenges and prospects of KA elimination.
As one of the neglected tropical diseases, KA is reported mainly from six countries namely Bangladesh, Brazil, Ethiopia, India, South Sudan and Sudan. In 2005, the Government of India, Nepal and Bangladesh signed a tripartite memorandum of understanding for the elimination of KA; later on Thailand and Bhutan also joined the group. Nepal is likely to achieve KA elimination soon.
Historically, dichlorodiphenyltrichloroethane (DDT) was used as an insecticide during the malaria eradication programme in India launched in 1953. As a result, KA was brought down to near eradication during the early 1960s. However, due to emergence of insecticide resistance in malaria vector, the DDT spray was discontinued in 1964. Thereafter, KA resurged with return of sand flies, leading to a big epidemic during the late 1970s, with 100,000 cases.
 The National Kala-azar Control Programme was initiated by the Government of India in 1990-1991 with sodium antimony gluconate (SAG) as the main drug used for the treatment of cases and DDT for vector control. The strategy for the national programme for the elimination of KA included early diagnosis and complete case management; integrated vector management and vector surveillance; supervision, monitoring, surveillance and evaluation; strengthening capacity of human resource in health; advocacy, communication and social mobilization for behavioural impact and inter-sectoral convergence; and finally programme management. The doses and duration of treatment with SAG were standardized in a study conducted in Bihar. During 1991-1992, there was an epidemic of VL in Bihar, India, with 250,000 cases. Dr Thakur’s clinic in Bihar started using amphotericin-B in 1991 for the treatment of SAG-resistant cases and also for fresh cases.
The National Kala-azar Control Programme was initiated by the Government of India in 1990-1991 with sodium antimony gluconate (SAG) as the main drug used for the treatment of cases and DDT for vector control. The strategy for the national programme for the elimination of KA included early diagnosis and complete case management; integrated vector management and vector surveillance; supervision, monitoring, surveillance and evaluation; strengthening capacity of human resource in health; advocacy, communication and social mobilization for behavioural impact and inter-sectoral convergence; and finally programme management. The doses and duration of treatment with SAG were standardized in a study conducted in Bihar. During 1991-1992, there was an epidemic of VL in Bihar, India, with 250,000 cases. Dr Thakur’s clinic in Bihar started using amphotericin-B in 1991 for the treatment of SAG-resistant cases and also for fresh cases.
Over time, KA cases in India have shown a decline from 24,212 with 93 deaths in 2009 to 8223 cases with nine deaths in 2015. KA cases in Bihar were 20,519 with 80 deaths in 2009 which decreased to 6280 with five deaths in 2015. In Muzaffarpur which was a heavily affected district of Bihar, 2308 cases of KA were reported with 11 deaths in 2009, which dropped to 711 with no death in 2015, in Jharkhand there were 20,875 cases of kala-azar with 12 deaths in 2009 which decreased to 1262 cases with no death in 2015.
 Considerable research has already been done in the country which provides insights into evolving situation of KA in the country as well as on its treatment and prevention aspects. For example, there is evidence that DDT, used initially for malaria elimination and manufactured in India, has become less effective or ineffective. Therefore, the practice of using DDT needs to be discontinued. Instead, newer insecticides such as pyrethroids or malathion should be used.
Considerable research has already been done in the country which provides insights into evolving situation of KA in the country as well as on its treatment and prevention aspects. For example, there is evidence that DDT, used initially for malaria elimination and manufactured in India, has become less effective or ineffective. Therefore, the practice of using DDT needs to be discontinued. Instead, newer insecticides such as pyrethroids or malathion should be used.
A new oral drug miltefosine which came in the market with a bang became less effective in a short span of time. Not only were there high number of relapse cases, but the cases of PKDL also increased after cure with miltefosine. The drugs which need to be used in this last phase of epidemic are amBisome and amphotericin-B.
In view of the changing scenario of KA in the country, the Ministry of Health and Family Welfare, Government of India and the State Governments need to work not only for case finding but also for curing these patients with effective drugs. The omission of KA in the priority list of diseases to be dealt by the government has raised a cause of concern.
The history of KA is older than the dated records. In those days malaria was very common and some epidemics of KA were passed as toxic malaria. The disease remained unrecognized for a fairly long time but the searching nature of human mind could come to a final diagnosis, though many aspects of the disease are still unexplored.
To achieve elimination of the disease, the Government should be ready to have a fortnightly review of KA situation and the experts need to visit the affected districts in highly affected states such as Bihar, Jharkhand and West Bengal, besides keeping a close watch on all the affected states. The search of cases should be both active and passive. Supervisory support should be provided to local doctors and private practitioners alike. Any case of fever of more than two weeks duration should be tested for kala-azar.
In the severely affected areas, active search for the KA cases could also be done. After due publicity patients with fever of more than two weeks duration should be asked to assemble at a common place. They should be examined for enlargement of spleen and liver, and tested for rk39 antibodies. Those found positive for anti-rk39 antibodies should be transferred to district hospitals or other secondary or tertiary care hospitals for further investigations for the confirmation of diagnosis.
The idea behind this system is that patients being the only source of infection are transferred away from the area as they can be the source of infection to others through sand flies. This method was found to be effective for elimination of KA in certain villages. The local ecology, environmental factors and climatic conditions such as temperature and rainfall can also play an important role in disease transmission and persistence.
 All these suggestions of Dr C P Thakur merit a serious consideration. He is currently a member of Rajya Sabha, a former minister in the Government of India, a physician and a leader of Bharatiya Janata Party. Having received a gold medal in M.B.B.S., he has obtained high qualification of M.D., M.R.C.P., and F.R.C.P. in the field of medicine. He went on to head the medicine department at Patna Medical College and conducted some of the most important research work in the country on KA, along with Dr Shyam Sundar from Benaras Hindu University.
All these suggestions of Dr C P Thakur merit a serious consideration. He is currently a member of Rajya Sabha, a former minister in the Government of India, a physician and a leader of Bharatiya Janata Party. Having received a gold medal in M.B.B.S., he has obtained high qualification of M.D., M.R.C.P., and F.R.C.P. in the field of medicine. He went on to head the medicine department at Patna Medical College and conducted some of the most important research work in the country on KA, along with Dr Shyam Sundar from Benaras Hindu University.
His suggestions on the latest KA trends have been accepted by the WHO and other international organizations and have been incorporated in various text books of medicine. The research on full moon and poisoning, published in BMJ (British Medical Journal) and other journals has attracted the attention of scientists all over the world. It has been abstracted in almost all the national daily newspapers, periodicals including Science Reporter.
Former Union Health Minister, Dr Thakur has been honoured with the first Prof S.C. Seal Memorial award for his contribution in the field of medicine. In 2017, he received a lifetime achievement award from the World Health Organization (WHO).
He was minister from 1999 to 2004 in the BJP government. He was born in 1933 in village Dubhah, Muzaffarpur district in Bihar. He received his degree from Patna Medical College, Patna University, Royal College of Physicians, London and Royal College of Physicians, Edinburgh and Royal College of Tropical Medicine and Hygiene, London.
He was elected to Lok Sabha from Patna constituency in 1984. Dr. C P Thakur has made a rather exceptional name in the city. He is one of the most renowned general physicians in the area. The credibility that this doctor enjoys in the medical field not only draws in patients from in and around the vicinity but from across the state as well.

Dr Thakur believes that the doctor’s reputation stems from the sheer passion to offer patients healthier living options. With the ever increasing and changing lifestyle, there is a need for windows to better treatment of diseases like Kala-azar. He possesses an impressive amount of knowledge and constantly keeps updated with advancements made in the medical field. Says the doctor with a healing touch, “Organizing a dependable mass health-care system is not easy in a country of the size of India. With progressive and, perhaps, inescapable privatisation of the health sector and the diminishing power of the state to mobilize large resources, there is the ever-present danger of marginalizing the poor.’’
The disease and the treatment
 Kala-azar is a chronic and potentially fatal parasitic disease of the viscera (the internal organs, particularly the liver, spleen, bone marrow and lymph nodes) due to infection by the parasite called Leishmania donovani.
Kala-azar is a chronic and potentially fatal parasitic disease of the viscera (the internal organs, particularly the liver, spleen, bone marrow and lymph nodes) due to infection by the parasite called Leishmania donovani.
Leishmania donovani, the agent of KA, is transmitted by sandfly bites. KA can cause no or few symptoms but typically it is associated with fever, loss of appetite (anorexia), fatigue, enlargement of the liver, spleen and nodes and suppression of the bone marrow. KA also increases the risk of other secondary infections. The first oral drug found to be effective for treating kala-azar is miltefosine.
Leishmaniasis is caused by a parasite that is spread to humans through the bite of infected sand flies. Leishmaniasis exists in many temperate and tropical countries of the world. The disease is most common in India especially Bihar, Jharkhand, Assam and West Bengal. Bangladesh, Nepal, Sudan, Ethiopia, Afghanistan, Algeria, Iran, Saudi Arabia, Syria, Brazil, Colombia, Peru, and Bolivia. The most common type of leishmaniasis is cutaneous leishmaniasis. This causes nodules or sores to form on the skin, including the skin of the face. Affected people may have a single lesion or many lesions. Sores heal slowly over months to years and leave scars.
Another type is called visceral leishmaniasis. Parasites infect the tissues of key organs, especially the liver, spleen, and bone marrow. Serious cases are usually fatal if not treated.
Uncommonly, people who have had cutaneous leishmaniasis may get new sores in the mucous membranes of the mouth, nose, and larynx even years after the cutaneous leishmaniasis has resolved. This is called mucocutaneous leishmaniasis and only occurs in limited areas.
Leishmaniasis is an infection caused by a parasite that is spread to people through the bite of the female phlebotomine sand fly. The parasite exists in many tropical and temperate countries. Cases in the United States are almost always imported from other countries by travelers or immigrants. Epidemics occur when people are displaced into affected regions through war or migration or when people in affected regions experience high rates of disease or malnutrition.
The major risk factor for leishmaniasis is being exposed to infected sand flies. The sand flies are most active after dusk and are more common in rural areas. Casual travelers do not usually visit these areas at night, so infection is more common in adventure travelers, Peace Corps workers, missionaries, soldiers, and those with occupational activities that require them to live in rural areas. In healthy people, the degree of immune response to leishmaniasis appears to be genetically determined. In visceral leishmaniasis, a weak immune response is associated with more severe disease.
Factors that weaken the immune system include malnutrition and infection with the human immunodeficiency virus (HIV). However, in mucocutaneous leishmaniasis, the symptoms appear to be caused in part by an overactive immune response. Interestingly, the Leishmania parasite itself can be infected with a virus that may cause the parasite to be more dangerous by overstimulating the inflammatory response from the human immune system.
It is important to remember that there are many diseases that can cause fever, weight loss, skin lesions, or enlargement of organs. Conditions like malaria, typhoid fever, toxoplasmosis, Chagas disease, schistosomiasis, tuberculosis, histoplasmosis, syphilis, and others may mimic some symptoms of leishmaniasis so a definitive diagnosis is essential.
Symptoms
A case of fever of more than two weeks duration not responding to anti-malarials and antibiotics. It means recurrent fever intermittent or remittent with often double rise of temperature.
Loss of appetite, pallor and weight loss with progressive emaciation
Weakness
Skin – Dry, thin and scaly and hair may be lost. Light coloured person show grayish discoloration of the skin of hands, feet, abdomen and face which gives the Indian name Kala-Azar meaning “Black fever”.
Anemia – develops rapidly
Splenomegaly – spleen enlarges rapidly to massive enlargement, usually soft and non-tender.
Liver – enlargement not to the extent of spleen, soft, smooth surface, sharp edge.
Causes
There is only one sand fly vector of Kala-Azar in India i.e. Phlebotomus argentipes. Sand flies are small insects, about one fourth of the size of a mosquito. The length of a sand fly body ranges from 1.5 to 3.5 mm.
Sand flies breed in high relative humidity, warm temperature, high subsoil water and abundance of vegetation. Sandflies breed in favourable micro-climatic conditions in places with high organic matter that serve as food for larvae. These are ecologically sensitive insects, fragile and cannot withstand desiccation.
Diagnosis and treatment
While treatment is lengthy and relatively costly, definitive diagnosis of KA requires tissue specimens, which are conventionally obtained by organ needle aspiration for microscopic demonstration of amastigote forms in stained smears.
Bone marrow, spleen, and lymph-node (in some regions) are the tissues most often sampled in patients with suspected infection. The diagnostic sensitivity of splenic aspiration is high, but the procedure carries a risk of bleeding; the sensitivity of examination of bone marrow specimens is considered to be lower. Organ aspiration and accurate examination of smears also require technical skills that are not uniformly available in rural areas. Culture or PCR testing of aspirate material improves parasitological yield, but these methods are seldom undertaken outside of research laboratories. There are no vaccines or preventive drugs for visceral leishmaniasis. The most effective method to prevent infection is to protect from sand fly bites. To decrease the risk of being bitten following precautions are suggested:
Outdoors:
1: Avoid outdoor activities, especially from dusk to dawn, when sand flies generally are the most active. When outdoors (or in unprotected quarters): Minimize the amount of exposed (uncovered) skin. To the extent that is tolerable in the climate, wear long-sleeved shirts, long pants, and socks; and tuck your shirt into your pants.
2: Apply insect repellent to exposed skin and under the ends of sleeves and pant legs. Follow the instructions on the label of the repellent. The most effective repellents generally are those that contain the chemical DEET (N, N–diethylmetatoluamide)
Indoors:
1: Stay in well-screened or air-conditioned areas.
2: Keep in mind that sand flies are much smaller than mosquitoes and therefore can get through smaller holes.
3: Spray living/sleeping areas with an insecticide to kill insects. If you are not sleeping in a well-screened or air-conditioned area, use a bed net and tuck it under your mattress.
4: If possible, use a bed net that has been soaked in or sprayed with a pyrethroid-containing insecticide. The same treatment can be applied to screens, curtains, sheets, and clothing (clothing should be retreated after five washings).

