Is it under diagnosed or over treated?

Gastro- Esophageal Reflux (GER) is a common but under-diagnosed condition in children. There is a low awareness about GER in children in India although the available data indicates that prevalence of GERD symptoms among Indian infants are almost the same as in Western infants. There are fundamental differences in the pathophysiology, clinical features, diagnostic evaluation and treatment in children and adults…….
By Dr. Neelam Mohan
Reflux is a physiological phenomenon occurring in every individual. Hence it is important to distinguish a benign and developmentally normal physiological event from a possible pathological GER. Most of neurologically normal children with GER have an excellent prognosis. Only children with ‘red flag ’signs require intervention.
Definitions
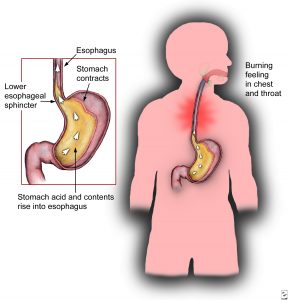
Regurgitation (spitting-up) is passage of refluxed gastric contents into the oral pharynx and mouth. Vomiting is defined as expulsion of the refluxed gastric content from mouth. Rumination is characterized by the voluntary, habitual regurgitation of recently ingested food that is subsequently spitted up or re-swallowed. Gastro-esophageal reflux is defined as involuntary passage of gastric contents in the esophagus. Gastro-esophageal reflux disease (GERD)-is defined by presence of reflux esophagitis and / or when it causes reflux symptoms that is sufficient to impair and/ or when it is associated with a risk of long term complications.
Clinical Presentations
| Table – I Symptoms related to reflux esophagitis |
| • Epigastric pain
• Heartburn • Non-cardiac chest pain • Dysphagia • Hematemesis /melena/ Anemia • Excessive crying/ irritability |
| Table –II : Extra-esophageal symptoms | ||
| Otorhinolaryngeal | Pulmonary | Others |
| • Chronic otitis media
• Chronic rhino-sinusitis • Hoarseness • Globus sensation • Persistent cough |
• Asthma
• Recurrent pneumonias • Persistent respiratory symptoms |
• Acute life threatening events
• Bradycardia • Abnormal posturing/ Sandifier’s syndrome • Dental erosions/ waterbrush |
Clinical features vary according to age of the children. In general, older children manifest gastro esophageal reflux disease similar to the adults. If regurgitation is associated with any ‘red flag ’signs like growth failure, acute life threatening events , apnea, stridor, recurrent pneumonia then they need evaluation and treatment. Older children usually present with heartburn, abdominal pain, regurgitation, dysphagia and complications such as Barrett’s esophagus, stricture. Their symptoms can be episodic with intermittent apparent disease free period.
Diagnostic Evaluation
As most infants and children with symptoms of GER are thriving and healthy, they require no diagnostic or therapeutic maneuvers other than a careful history and physical examination, with appropriate reassurance to the parents if anxiety is present. Infants and older children who have significant neurologic deficits or psychomotor retardation often have significant GER and may suffer from serious sequelae secondary to GER.
In most adolescents with regurgitation and heartburn, a good history and physical examination are usually sufficient to diagnose GERD, recognize complications, and initiate treatment. Further diagnostic testing is required only in patients with symptoms of odynophagia, dysphagia, upper gastrointestinal bleeding, weight loss, atypical chest pain, respiratory disease or an inadequate response to empiric therapy. Patient with these alarm signs require endoscopic evaluation or evaluation directed at exclusion of other causes of these symptoms.
Diagnosis
A good history is mandatory for the diagnosis of GERD. There is no role of barium swallow in diagnosis of GERD. Technetium Scan is usually done in infancy. It has a sensitivity of 55%-80% and is good to pick up pulmonary aspiration. UGI endoscopy and biopsy is indicated for persist end symptoms and is also useful in ruling out other differentiate diagnosis such as allergic enteropathy. 24 hrs impedance pH metry is the gold standard and is ideal for atypical symptoms.
Pharmacologic Management:
If conservative measures fail and other differential diagnosis have been considered and excluded, pharmacological therapy is warranted. One algorithm allows for a trial of medical therapy before any diagnostic evaluation is performed. If the patient improves with the use of medications, no further evaluation is necessary. However, if no improvement occurs, a diagnostic work-up should be performed. It is debatable whether medical therapy should be initiated before diagnostic evaluation or vice-versa. The pharmacological therapy includes prokinetics and antacids and agents that suppress gastric and production like H2 receptor antagonists and proton pump inhibitors.
Histamine-2 receptor antagonists (H2RAs) decrease acid secretion by inhibiting histamine-2 receptors on gastric parietal cells. Gastric pH begins to increase within 30 minutes of administration and the effect lasts for 6 hours.. Advantage of H2RAs is its quick action and its causes partial block in acid secretion. It’s best for mild to moderate cases. However tachyphylaxis, or diminution of the response and escape from its acid-inhibitory effect have been observed after 6 weeks
PPIs inhibit acid secretion by blocking Na–K- ATPase, the final common pathway of parietal cell acid secretion, often called the proton pump. PPIs produce higher and faster healing rates for erosive esophagitis than H2RAs. The superior efficacy of PPIs is largely because of their ability to maintain intragastric pH at or above 4 for longer periods and to inhibit meal-induced acid secretion, a characteristic not shared by H2RAs. The most common side effects include headache and diarrhea, rarely decrease in serum vitamin B12 levels. Unnecessary use of PPI should be avoided as long term renal concerns are with reported in the recent time.
Surgery: An alternative treatment in patients who have chronic reflux with recalcitrant symptoms includes antireflux surgery, including open and laparoscopic versions of Nissen fundoplication. Some of the common indications for surgery are failed medical management, patient preference for surgery despite successful medical management, complications of GERD, medical complications attributable to a large hiatal hernia, or atypical symptoms with reflux documented on 24-hour pH monitoring . Candidates for surgery should normal esophageal motility by manometry. Postsurgical complications are common like 10% having solid food dysphagia and 7 to 10% of patients have gas bloating but these are manageable.
(The author is Director and HOD, Department of Pediatric Gastroenterology, Hepatology & Liver Transplantation, Medanta Superspeciality Hospital, Gurgaon)

