Let Your Heart Stay Healthy

To curb the increasing incidence of coronary artery disease among younger people, it is vital for them to adopt lifestyle changes and stay away from risk factors such as smoking, obesity, diabetes, and dyslipidaemia or abnormal cholesterol levels….
By Dr Manoj Kumar Rohit
Coronary artery disease that is, the disease affecting the arteries of the heart, is one of the leading causes of mortality in the world. Commonly referred to as the disease of older people, its occurrence in Indians is seen approximately one decade earlier than the western population. Moreover, its incidence is on the rise in the last three decades especially among the urban population.
Coronary heart disease, in general, can be attributed to four causes:
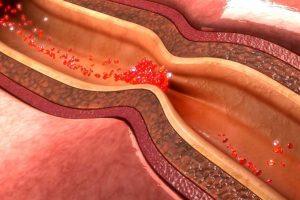
Atheromatous coronary artery disease (Deposition of cholesterol in the coronary arteries)
Non-atheromatous coronary artery disease (Includes other abnormalities such as coronary artery spasm, coronary artery dissection, coronary artery aneurysms)
Hypercoaguable states (Genetic causes increasing the predisposition to clot formation)
MI related to substance abuse (Especially cocaine abuse and binge alcohol consumption emerging as risk factors)
Premature coronary artery disease is defined as cardiac disease occurring in younger age groups < 45 years of age. The incidence of CAD in young population of India is higher when compared to rest of the world and comprises about 15% of all the CAD patients. The vulnerability of Indians to myocardial infarction may be related to lifestyle, environmental and genetic factors.
Numerous risk factors are associated with coronary artery disease and almost 85% to 90% of the disease can be attributed to conventional risk factors. The increasing prevalence of smoking, obesity and diabetes especially in the young population predisposes them to heart disease. Dyslipidemia or abnormal cholesterol levels can be attributed to both environmental and genetic causes, thus people with strong family history tend to have a higher chance of developing cardiac diseases in early stage of life as compared to those without. Physical inactivity, lack of exercise and stress are other overlooked factors which contribute significantly. Cocaine abuse is an emerging risk factor which can cause the arteries to go into spasm and cause myocardial infarction.
Other causes of CAD which play an important role especially in young patients include congenital abnormalities of the coronary arteries, childhood Kawasaki disease, coronary artery dissection especially seen in postpartum females, presence of hypercoagulable states and coronary artery spasm.
The presentation of myocardial infarction in younger population also may not be typical. Many patients do not report any previous history of angina pain, and first episode often leads to fully evolved MI in a short span of time. Rapid progression combined with low index of suspicion may often delay the presentation to the hospital thus losing on the precious time.
 The disease once diagnosed carries a significant morbidity, mortality and psychological impact on the concerned individuals and his family. Better prognosis is achieved with timely diagnosis, investigation and treatment. Any patient with chest pain and suspected cardiac disease should be referred to specialist early and scope of early coronary angiography and intervention should be assessed.
The disease once diagnosed carries a significant morbidity, mortality and psychological impact on the concerned individuals and his family. Better prognosis is achieved with timely diagnosis, investigation and treatment. Any patient with chest pain and suspected cardiac disease should be referred to specialist early and scope of early coronary angiography and intervention should be assessed.
MI in younger patients carries a better prognosis if assessed and treated on time. Apart from regular dose of blood thinners and cholesterol lowering medications, control of risk factors plays an important role in management of these patients. Stopping smoking should be strongly advised. Good control of diabetes, regular exercise with correction of lipid abnormalities improves the prognosis in patients.
Study conducted in PGIMER revealed high prevalence of young patients with myocardial infarction. The risk factors included male sex, smoking, dyslipidaemia, heavy alcohol consumption and strong family history. Delay in seeking treatment is often the cause for poor prognosis. Early management with lifestyle changes often leads to better results
 Main Findings of PGI study on young heart patients
Main Findings of PGI study on young heart patients
All patients presenting to Coronary Care Unit (CCU), Department of Cardiology, Post Graduate Institute of Medical Education and Research (PGIMER) fulfilling the inclusion criteria and not meeting the exclusion criteria were eligible for the enrolment. Our study included all cases of young (<40yrs) acute coronary syndrome patients falling in the inclusion criteria and presenting to CCU, department of cardiology. The study was conducted over a period of one and a half years.
A total of 182 young patients with ACS were included in the study. 96.2% were males and 3.8% were females. 21.4% were from upper socioeconomic status and 78.6% were from lower socioeconomic status. Roughly half were from rural areas and other half from urban areas
Smoking, alcohol consumption, hypertension, family history of premature CAD, diabetes mellitus, physical inactivity, prior history of CAD and history of CVA were the major risk factors in the study
Elevated plasma homocysteine, elevated serum lipoprotein (a), elevated serum triglycerides, LDL, total cholesterol and low HDL were other risk factors seen in young patients with ACS in our study
Only 4.4% presented to the nearest hospital on time. None presented to PCI capable hospital within 30 minutes. Only 6.6% presented to PCI capable hospital within 120 minutes. Prehospital factors were the main reasons for delay in presentation to hospital.
Majority of the study population did not consider symptoms to be serious, most patients exhibited pain resistance behaviour and misinterpreted the nature of pain.
Majority of study population were living in a distance farther from hospital and lacked suitable transportation.
Angina was the most common symptom followed by dyspnea and atypical chest pain among the study population.
STE-ACS was more common than NSTE-ACS. Most common diagnosis made was AWMI (57.7%) followed by IWMI (22.5%), NSTE-ACS (18.1%) and LWMI (1.6%)
Median time to first medical contact among study participants was 300 (10-43200) minutes. Median time to transportation to PCI capable hospital was 1440 (60-86400). Mean pain to needle time was 257.3±152.5 minutes and median pain to balloon time was 2880 (75-68400) minutes
Majority of the population underwent coronary angiography. 26.8% of the population who underwent coronary angiography had insignificant CAD and 73.2% had significant CAD.
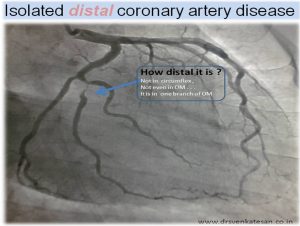
SVD was more common followed by DVD, TVD and LM disease. Thrombotic lesions were found in 1/4th of the study population. LAD was the most common vessel involved followed by LCX and RCA.
7.2% were diagnosed with MINOCA, 4.2% had CSFP, 4.2% had SCAD and 1.2% had coronary artery ectasia.
6.6% had cardiogenic shock. 8.8% had left ventricular failure. 2 patients had complete heart block which reverted to sinus rhythm with revascularisation. 2 patients had Bifascicular block. Primary VT occurred in 2.2% of study population.
2 patients had LV apical clot out of which 1 patient developed cardioembolic stroke.
42.3% underwent thrombolysis. Streptokinase was the most common thrombolytic agent used followed by Reteplase and Tenekteplase.
54.3% underwent revascularisation. 96% of revascularisation group underwent PCI, 2% underwent CABG
Only 3% underwent primary PCI, 3.6% underwent rescue PCI. 92% underwent only culprit vessel PCI, 12.1% underwent both culprit and non-culprit vessel PCI. This trend is probably due to late presentation to our centre after initial symptoms.
1 patient had coronary perforation during revascularisation and 1 patient had acute stent thrombosis
Patients with cardiogenic shock and left ventricular failure had prolonged in-hospital stay and had higher TIMI score, Killip class. Patients with cardiogenic shock and left ventricular failure had lower ejection fraction
There was no in-hospital mortality, 1 patient died on follow up due to ADHF and cardiogenic shock. 4 patients had ADHF on follow up.
Conclusion: This prospective study in young patients with ACS indicates that the conventional risk factors continue to be the major cause of CAD in the young. There is urgent need to focus on these risk factors in primary and secondary prevention. Screening for risk factors should start at an early age in Indian males and cessation of smoking, promotion of physical activities should be encouraged. Optimal control of hypertension, diabetes and dyslipidaemia should be undertaken.
All young ACS patients should be screened for hyperhomocysteinemia. Delay in seeking treatment for ACS symptoms is still a problem, with pre-hospital delay times being constantly high. Failure to recognize the importance of symptoms, lack of transportation is very prevalent. Reperfusion strategies are underutilized.
Proper education and EMS facilities should be made available to general population to reduce these delays in seeking treatment. Coronary artery disease is less severe among young ACS patients. Around 1/4th of population has insignificant CAD. ACS in less than 40 years of age is almost exclusively a disease seen in males. Anterior wall MI is more common and most of the patients have single vessel disease. In hospital mortality is very low in this young population.
(The author is Professor and Incharge, Cardiology Unit II, Department of Cardiology, Advanced Cardiac Centre, Post Graduate Institute of Medical Education & Research, Chandigarh)

