Coping with the Pause

Navigating menopause requires candid conversations along with knowledge, support, and empowered health. Latest medical breakthroughs, holistic wellness strategies, and growing awareness are gradually reshaping how we view this natural process in a woman’s life
By Dr Suneela Garg
Menopause represents the natural and permanent stoppage of menstruation, a transition that marks the end of a woman’s reproductive years. It is clinically defined as occurring after 12 consecutive months without a menstrual period, stemming from the depletion of ovarian follicles and a consequent decline in oestrogen and progesterone production. This biological shift is a universal experience yet its personal and societal implications are undergoing a profound re-evaluation.
Once shrouded in silence, menopause is now emerging as a critical public health, economic, and social equity issue, demanding informed dialogue and compassionate, personalised care.
The Biology of the Transition
At its core, menopause is a hormonal milestone. The ovaries, having depleted their supply of follicles that contain immature eggs, significantly reduce their production of the hormones oestrogen and progesterone. This decline is not an abrupt event but a process, often beginning years before the final period in a phase known as perimenopause or the menopausal transition.
Natural menopause typically occurs between the ages of 45 and 55, with the median age being around 51 in the United States. In India, the average age is notably younger, at approximately 46.2 years. However, variations exist, and menopause is classified as premature if it occurs before the age of 40, and early if before 45. This stage of life can also be induced surgically through the removal of both ovaries (oophorectomy) or medically by treatments like chemotherapy or pelvic radiation.
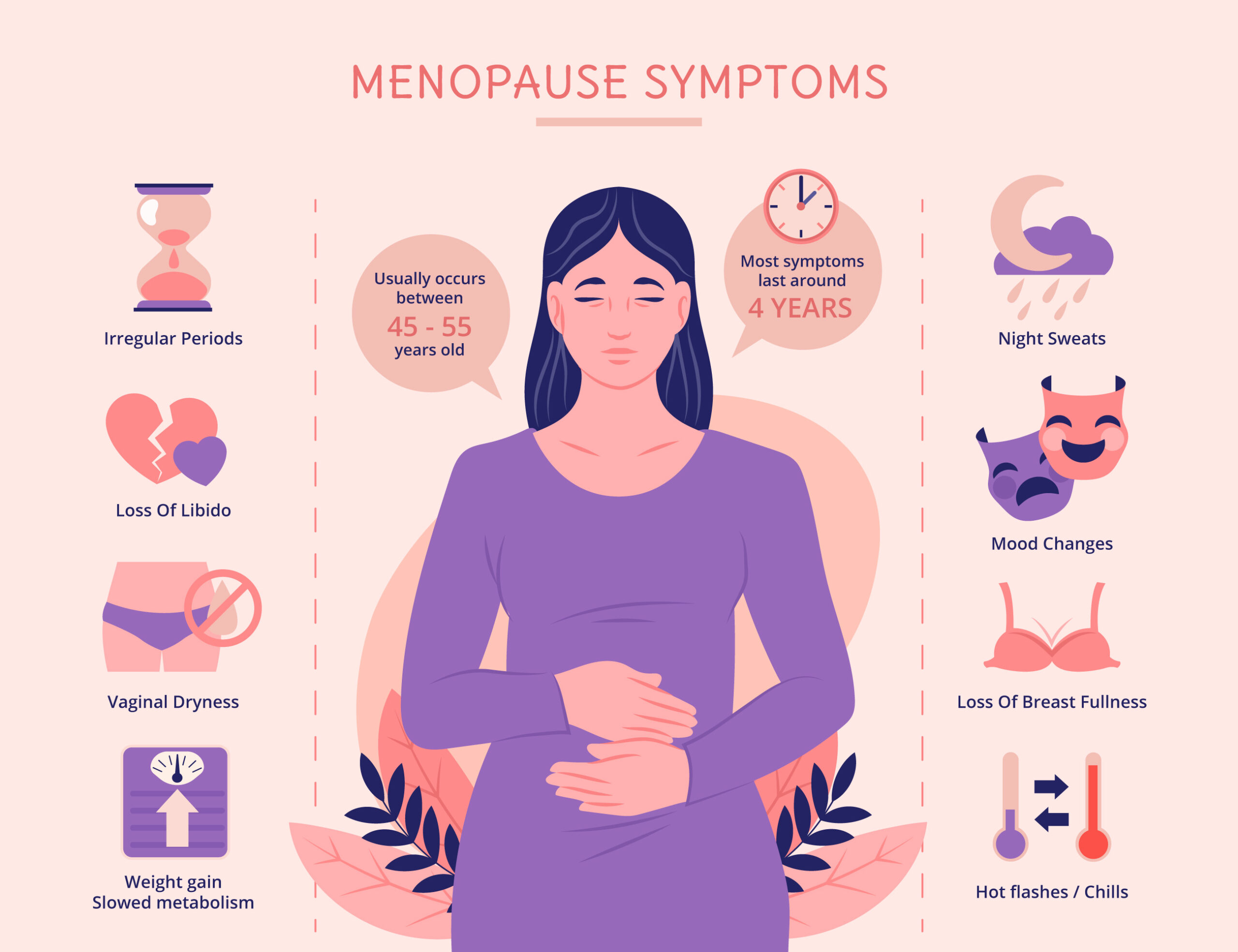
Recognising the Spectrum of Symptoms
The drop in hormone levels triggers a wide array of symptoms that extend far beyond the commonly known hot flashes. Vasomotor symptoms, which include sudden feelings of intense warmth (hot flashes) often accompanied by sweating and flushing, are indeed a hallmark. When these occur at night, they are termed night sweats and can severely disrupt sleep. Menstrual cycles become irregular in frequency, duration, and flow before stopping altogether.
Beyond these, the symptom profile is broad. Many women experience sleep disturbances, mood changes like irritability, anxiety, or depression, and cognitive effects sometimes called “brain fog.” Physical changes include vaginal dryness, which can lead to discomfort during intercourse; urinary issues like incontinence or increased frequency; joint and muscle aches; skin changes; and shifts in libido. The severity and combination of these symptoms vary greatly from one woman to another, influenced by genetics, overall health, and lifestyle.
Long-Term Health Considerations
The impact of menopause extends beyond immediate symptoms, influencing long-term health due to the protective role oestrogen plays in various body systems. The decline in oestrogen is associated with an accelerated loss of bone density, increasing the risk of osteoporosis and fractures. It also contributes to changes in cholesterol levels and blood vessel function, elevating the risk of cardiovascular disease—the leading cause of death in postmenopausal women. These systemic effects underscore why menopause management is not merely about symptom relief but is integral to lifelong health and active aging.
Menopause as a Societal Imperative
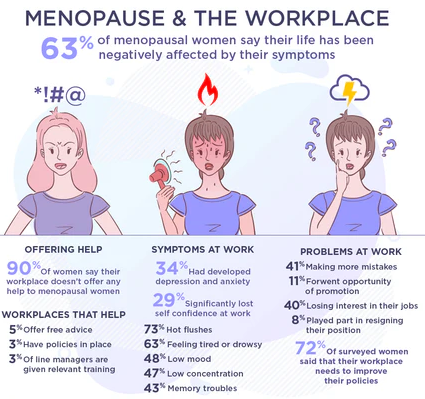
For generations, menopause was a taboo subject, burdened by a combination of ageism, sexism, and a stark lack of education. This silence forced many women to navigate challenging symptoms with embarrassment and without adequate support, negatively impacting their mental health, careers, and quality of life. Today, a significant shift is underway. Increased public discourse, advocacy by public figures, and media attention are helping to normalise the conversation.
This growing awareness has catalysed its recognition as a serious workplace and economic issue. Surveys indicate that severe, unmanaged symptoms lead many women to consider reducing work hours, declining promotions, or taking early retirement. In the United States alone, the annual economic impact from missed workdays is estimated at $1.8 billion. In response, progressive organisations are beginning to implement menopause-friendly policies, such as flexible working hours, temperature-controlled environments, and manager training, acknowledging that supporting employees through this transition is both a moral and economic imperative.

The conversation is also becoming more inclusive. The World Health Organization (WHO) acknowledges that transgender men and gender-diverse people may also experience menopause, broadening the scope of care and understanding. Furthermore, cultural perspectives are being recognised; research shows symptom experience can vary across populations. For instance, some studies suggest Asian women report fewer vasomotor symptoms than Western women, highlighting the need for culturally competent care that respects diverse experiences and traditional wellness practices like Ayurveda.
Advances in Treatment and Management
The medical approach to menopause has evolved significantly, moving towards personalised, evidence-based strategies. A key area of progress is the nuanced re-evaluation of Menopausal Hormone Therapy (MHT), once known as Hormone Replacement Therapy (HRT). Following the 2002 Women’s Health Initiative study, which highlighted potential risks, MHT use plummeted. However, subsequent analysis has provided a more balanced view. It is now understood that for many healthy women under 60 or within 10 years of menopause onset, MHT is a safe and effective option to relieve debilitating symptoms and protect bone health. In a significant development, an FDA panel in July 2025 called for the removal of strict “black box” warnings on certain MHT products, arguing that excessive fear has deprived many women of beneficial treatment.

For those who cannot or prefer not to use hormones, new non-hormonal options are available. In 2023, the US Food and Drug Administration (FDA) approved fezolinetant (Veozah), the first drug designed specifically to target the brain’s neural pathways that trigger hot flashes and night sweats. Preliminary Phase 4 data released in October 2025 showed that fezolinetant significantly improved sleep, work productivity, and overall quality of life.
Increasingly, the foundation of management is holistic lifestyle medicine, encapsulated by the 2025 World Menopause Day theme “Lifestyle Medicine.” The International Menopause Society emphasises a core protocol: a balanced diet rich in calcium and vitamin D; regular weight-bearing and resistance exercise to maintain bone and muscle mass; stress-reduction techniques like cognitive behavioural therapy (CBT), meditation, or yoga; and prioritising sleep hygiene. This integrative approach empowers women to build resilience from within.
Understanding Premature and Early Menopause
The trend of menopause occurring before age 45 is a growing concern. The causes are multifaceted. Genetic factors play a role, including conditions like Turner syndrome or a family history of early menopause. Autoimmune diseases, where the body’s immune system attacks the ovaries, can be a trigger. Medical interventions such as chemotherapy, radiation to the pelvic area, or surgical removal of the ovaries induce immediate menopause. Lifestyle factors, particularly smoking, are strongly linked to an earlier onset, as may be exposure to certain environmental toxins. In some cases, no specific cause is identified, a condition known as Primary Ovarian Insufficiency (POI).
Early menopause carries significant implications, particularly for fertility and long-term health. It extends the duration of low oestrogen exposure, potentially heightening the risks for osteoporosis, cardiovascular disease, and neurological changes. This makes timely diagnosis, supportive counselling, and proactive health management even more critical for this group.
Dispelling Common Myths
Misinformation about menopause persists, creating unnecessary anxiety. It is a myth that menopause happens suddenly; it is a gradual transition through perimenopause, which can last several years. Another common misconception is that pregnancy is impossible during perimenopause; however, ovulation can still occur erratically, and contraception is advised until menopause is confirmed. The belief that MHT/HRT is universally dangerous is outdated; its benefits and risks are individual and must be evaluated with a healthcare provider.
While the average age is in the late 40s, menopause can affect younger women. Finally, the idea that menopause ruins one’s sex life is false; while vaginal dryness may occur, it is treatable, and many women report renewed sexual freedom post-menopause.
The Indian Context and Holistic Pathways
In India, with an average menopause age of 46.2, the conversation is vital. Factors like lifestyle changes, urban stress, and lower awareness can exacerbate symptoms and delay help-seeking. Here, traditional systems like Ayurveda offer complementary pathways, focusing on holistic balance through diet (Aahara), lifestyle (Vihara), herbal medicine (Aushadhi), and therapies (Karma). Herbs such as Ashwagandha for stress adaptation, Shatavari for female rejuvenation, and Amla for vitality are traditionally used to support the body’s transition. An Ayurvedic diet emphasises warm, nourishing foods, phytoestrogen-rich plants like soy and flax seeds, and the avoidance of excessive caffeine, spice, and processed foods. Practices like yoga and pranayama (breathing exercises) are recommended to balance the body’s energies (doshas) and promote mental calm.

A Roadmap for a Smoother Transition
Navigating menopause successfully is an active process. Open communication with healthcare providers is the first step to creating a personalised management plan. This may include discussing the suitability of MHT, exploring new non-hormonal medications, or receiving guidance on bone density and heart health screenings.
Building a daily routine that incorporates regular exercise, a nutrient-dense diet, dedicated stress management, and good sleep hygiene forms the bedrock of wellbeing. Seeking support, whether from understanding friends and family, workplace accommodations, or dedicated support groups, alleviates the emotional burden.
It is empowering to reframe menopause not as a disease, but as a natural and manageable stage of life. With growing research, evolving treatments, and a breaking silence, women today have more resources than ever to navigate this transition with knowledge, support, and grace. It paves the way for decades of healthy, vibrant postmenopausal life.
(The author is Professor of Excellence, Community Medicine; Former Sub-Dean, Maulana Azad Medical College (MAMC), New Delhi; and Chairperson, Programme Advisory Committee, National Institute of Health and Family Welfare, Delhi.)

