A Growing Epidemic
 Chronic Kidney Disease is projected to become the fifth leading cause of death by 2040 if left unchecked. The tragedy is not the inevitability of the disease, but the neglect of the very tools that could stop it: timely detection and a new generation of therapies that can halt the disease in its tracks.
Chronic Kidney Disease is projected to become the fifth leading cause of death by 2040 if left unchecked. The tragedy is not the inevitability of the disease, but the neglect of the very tools that could stop it: timely detection and a new generation of therapies that can halt the disease in its tracks.
By Dr Sanjeev Gulati
In the quiet, unseen corridors of our bodies, a silent and relentless epidemic is advancing. Chronic kidney disease (CKD), a condition once perceived as a rare and specialised medical concern, has burgeoned into one of the most common and yet most dangerously overlooked public health crises of our time. The statistics are stark and speak to a profound failure of early detection: despite significant progress in medical science, mortality attributed to kidney disease continues its inexorable climb year after year. Current projections deliver a sobering forecast—by the year 2040, CKD is poised to become the fifth leading cause of death globally. This is not a distant threat; it is a present reality unfolding within our communities, often unnoticed until it is tragically too late.
The scale of the problem within India is particularly jarring. A comprehensive, population-based screening study orchestrated by the Indian Society of Nephrology, encompassing 50,000 individuals across the nation, has illuminated a truth we can no longer ignore. The data reveals that between 20 and 30 out of every 100 adults in our country are now living with some degree of chronic kidney disease. Perhaps the most alarming facet of this finding is that the vast majority of these individuals are entirely unaware of their compromised renal health. This represents a prevalence rate of nearly one-quarter of the adult population, a figure that signifies not merely a medical statistic but a silent tide of suffering and future healthcare burden that threatens to overwhelm our systems.

Understanding the nature of CKD is the first step towards combating it. It is a classic example of a progressive condition. It begins quietly at stage one, with minimal, often imperceptible damage, and advances methodically through subsequent stages. Left unchecked, it culminates in stage five, known as end-stage renal disease, where the kidneys have lost nearly all their ability to function. The significant message of modern nephrology, however, is that this progression is not an inevitability. The trajectory of the disease can be dramatically altered, and even arrested, provided it is identified in its formative stages. The window of opportunity lies in stages one to three, where timely and sustained intervention can preserve kidney function for decades, allowing individuals to live full lives without ever facing the spectre of dialysis.
The gateway to this early intervention is disarmingly simple and rests upon two fundamental tests that should be as routine as checking blood pressure. The first is the urine albumin-creatinine ratio, a test designed to detect microalbuminuria—the presence of minute, abnormal amounts of the protein albumin in the urine. This is the earliest biochemical sign of kidney distress, a signal that often manifests long before traditional markers like serum creatinine begin to rise. The second is the estimated glomerular filtration rate, calculated from a simple blood test for creatinine alongside the patient’s age and sex, which provide a measure of how efficiently the kidneys are filtering waste from the blood.

The profound value of identifying microalbuminuria extends beyond the kidneys; it is also a well-established and powerful marker for heightened risk of cardiovascular disease. Thus, a single positive test serves a dual purpose: it sounds the alarm for kidney protection and flags the need for a thorough cardiac assessment.
The implementation of widespread screening is both feasible and critical. Our own community-based research has demonstrated that initial screening for microalbuminuria can be achieved through a straightforward, point-of-care urine dipstick test, ideal for use in primary health centres and community camps. A positive result should then be followed by a confirmatory laboratory assessment of the albumin-creatinine ratio alongside eGFR measurement. Establishing a National Kidney Screening Programme founded on this simple protocol would represent a monumental leap forward in proactive public health, moving us from a paradigm of late-stage treatment to one of early preservation.
The past decade has witnessed nothing short of a revolution in our ability to protect the kidneys once early damage is identified. We have moved far beyond the era where treatment was limited to controlling blood pressure with medications like angiotensin-converting enzyme inhibitors. Today, we possess a sophisticated and growing therapeutic arsenal designed to shield the kidney directly.
The emergence of SGLT2 inhibitors, such as dapagliflozin and empagliflozin, has been transformative. Originally developed for diabetes management, these drugs have proven to offer extraordinary kidney and cardiovascular benefits, significantly slowing the progression of CKD and reducing heart failure events regardless of diabetic status.
Furthermore, the recent introduction of finerenone, a selective mineralocorticoid receptor antagonist, provides a targeted weapon against the inflammation and scarring that drives diabetic kidney disease. These modern pharmaceuticals represent a profoundly cost-effective strategy. Their expense is negligible when weighed against the colossal human and financial cost of managing end-stage kidney failure with lifelong dialysis or transplantation. Investing in early, effective pharmacotherapy is an investment in a healthier population and a more sustainable healthcare future.
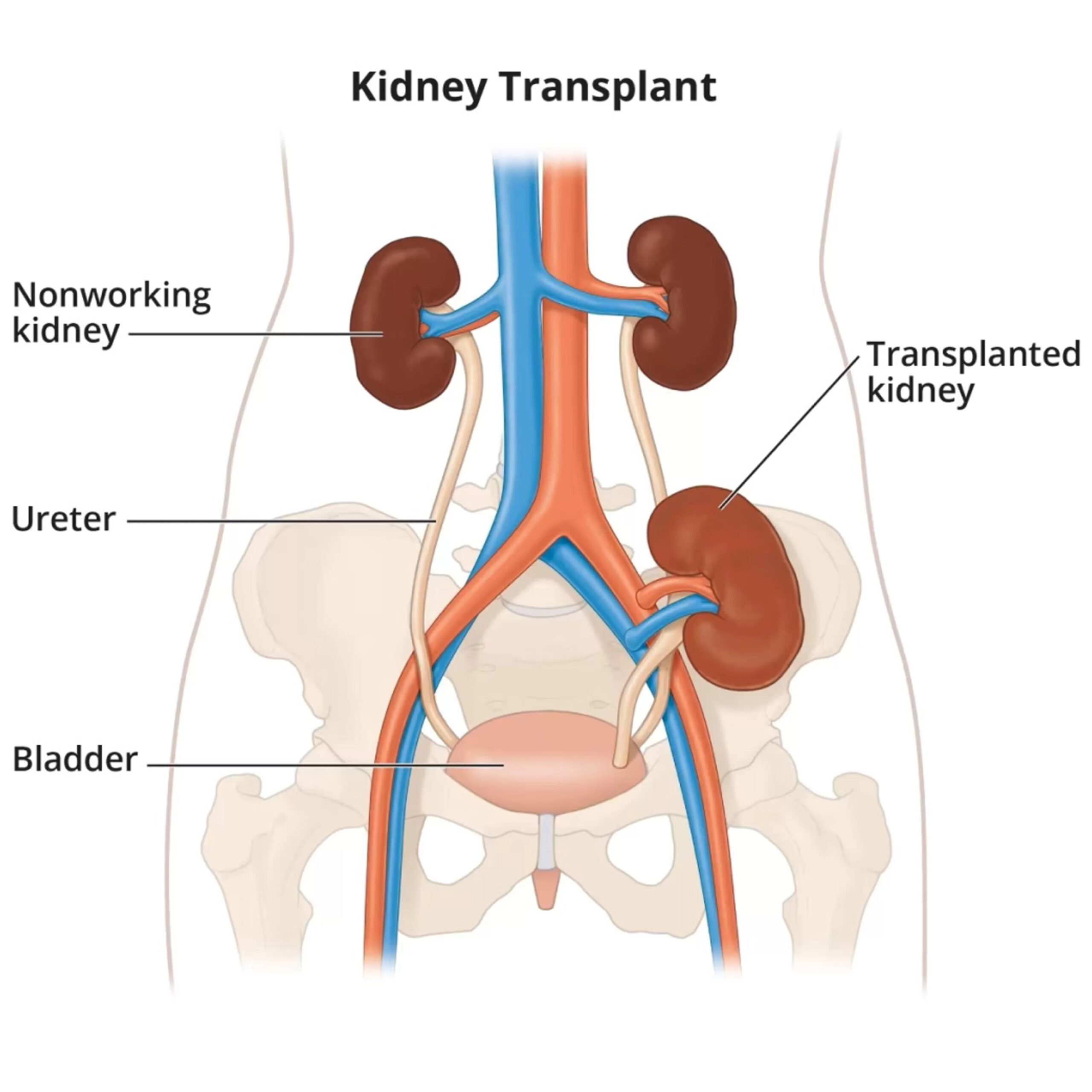
When prevention and early intervention are unsuccessful, and CKD progresses to its final stage, patients and their families face a daunting crossroads. At stage five, the options narrow to two life-sustaining treatments: dialysis or kidney transplantation. It is a moment that demands clarity and caution, as vulnerable patients are often targeted by misinformation promoting unscientific and invalidated “alternative” cures.

The reality is stark—there are no alternatives. Dialysis, while a life-saving procedure, is a demanding and burdensome therapy that typically requires attending a hospital or clinic three to four times a week for several hours each session, indefinitely.
The evidence overwhelmingly supports kidney transplantation as the superior treatment for eligible patients. The contrast in outcomes is dramatic. In India, where organ donation rates remain regrettably low, the one-year survival for patients on dialysis is approximately 75 per cent, a figure that plummets to a mere 20 per cent at five years. These individuals also face a significantly diminished quality of life, with frequent hospitalisations for infections or cardiac complications, and an enduring dependency that affects every aspect of their existence. In stark contrast, the one-year survival rate following a successful kidney transplant exceeds 99 per cent.
At five years, patient survival remains above 95 per cent, with the transplanted kidney itself functioning well in about 80 per cent of cases. Beyond the statistics, a successful transplant offers the priceless gift of restored freedom. It allows a person to return to work, to education, to travel, and to engage fully in family and social life. They transition from being a dependent patient to a contributing member of society. This is why the medical community strongly advocates for pre-emptive kidney transplantation—receiving a transplant before ever needing dialysis—whenever possible, as it is associated with the very best long-term outcomes for both the patient and the graft.
The ultimate strategy, however, will always be to prevent CKD from taking root in the first place. The lifestyle choices that safeguard our kidneys are the very same ones that protect our hearts and our overall metabolic health—a truly beneficial synergy.
Foremost among these is the avoidance of tobacco in any form, as smoking causes direct damage to the intricate vascular network within the kidneys. Maintaining a healthy weight is paramount, as obesity is a primary driver of both hypertension and type 2 diabetes, the two leading causes of CKD. A balanced diet, low in processed salts, saturated fats, and refined sugars, and rich in whole foods, provides the foundation for renal health.
Regular physical activity, whether it is a daily half-hour walk or the disciplined practice of yoga, which also serves as an excellent stress reliever, improves metabolic control and circulation. Staying well-hydrated with water, while strictly moderating alcohol intake, supports kidney function. Additionally, public awareness must include caution regarding the unsupervised, chronic use of common pain medications like non-steroidal anti-inflammatory drugs, which can inflict significant kidney damage over time.

Confronting the silent epidemic of chronic kidney disease demands a coordinated and compassionate response on a national scale. It requires a three-pronged approach: first, a concerted public health campaign to raise awareness and implement widespread screening; second, the integration of modern, kidney-protective therapies into standard primary care; and third, a sustained effort to promote healthy living from an early age. Bridging the profound knowledge gap that currently exists is the essential step. For in the battle against this insidious disease, knowledge is indeed more than power—it is the very key to prevention, to preservation, and to a future where the forecast of rising mortality can be decisively reversed.