Elevating Healthcare Safety

Healthcare facilities stand as the first line of defence against infectious diseases. The Consortium of Accredited Healthcare Organisations (CAHO) focuses on comprehensive measures to minimise infection risks and enhance public health outcomes.
By Dr Malathi Murugesan
Healthcare facilities play a crucial role in infection prevention and control (IPC), serving as frontline defences against the spread of infectious diseases among patients, bystanders, and healthcare workers. Their role encompasses a range of measures aimed at minimising the risk of infections. Most importantly, a dedicated infection control committee with key experts should be established in all healthcare facilities to constantly monitor and support the system.
The main aim of this committee is to develop stringent protocols and guidelines to prevent the transmission of infectious agents. These include hand hygiene practices, proper sanitation of medical equipment, and the use of personal protective equipment (PPE) such as masks, gloves, and gowns. Once the guidelines are established according to the hospital’s requirements, the committee needs to continuously monitor and track infectious diseases within their premises. This involves surveillance of patient populations, tracking trends in infection rates, and identifying outbreaks early to implement effective and timely control measures.
The infrastructure should be equipped with facilities that establish isolation units to contain patients with contagious diseases, preventing further spread. Facilities must maintain clean and hygienic environments through regular cleaning and disinfection of surfaces, equipment, and patient care areas. Proper heating, ventilation, and air conditioning systems (HVAC) are required for controlling airborne pathogens and maintaining indoor air quality, which was found to have a crucial impact during the COVID-19 pandemic.
Healthcare facilities must actively promote and administer vaccinations to prevent the spread of vaccine-preventable diseases (VPD) among patients, staff, and the community. Vaccination programs are essential for achieving herd immunity and reducing the incidence of infectious diseases. Each hospital should have a vaccination policy tailored to the needs of vulnerable populations. These protocols and policies need to be effectively communicated through comprehensive education and training programs for healthcare workers. This includes training on proper hand hygiene techniques, the use of personal protective equipment (PPE), and adherence to infection prevention and control protocols. Establishing effective communication channels is crucial for disseminating information, sharing best practices, and responding promptly to emerging infectious threats.

Burden of Infectious Diseases
According to data from the Global Burden of Disease Study 2019, 60% of the communicable disease burden among children and adolescents is attributed to enteric infections (69.5 million Disability Adjusted Life Years [DALYs]), lower respiratory tract infections (LRTIs; 64.7 million DALYs), and malaria (38.3 million DALYs).
In India, accurate estimates of the burden of healthcare-associated infections (HAI) are hindered by the absence of reliable and routinely standardised surveillance data. Published reports of healthcare-associated infections mostly originate from individual tertiary care health facilities. These reports typically comprise short-term prospective studies and point prevalence surveys conducted within selected study populations. A recent landmark study from India was published, detailing data from a network of 26 tertiary-level hospitals. This network was established to implement healthcare-associated infections surveillance and prevention activities. The study reported 2,622 healthcare-associated bloodstream infections and 737 healthcare-associated urinary tract infections (UTIs) from 89 intensive care units (ICUs) between May 2017 and October 2018.
Given these gaps in estimates, along with a lack of awareness in infection prevention and control and insufficient support system/budget allocation for various activities such as biomedical waste management, vaccination, and procurement of disinfection agents, it is imperative to undertake a nationwide initiative.
Role of Consortium of Accredited Healthcare Organisations (CAHO) in IPC activities
CAHO plays a crucial role in infection prevention and control (IPC) activities within the healthcare sector. As a not-for-profit organisation, CAHO represents healthcare institutions, diagnostic centres, and quality professionals, aiming to promote patient safety through comprehensive training programs for healthcare professionals. These programs encompass various domains including quality, communication, and accreditation standards.
One of CAHO’s key strengths lies in its network of eminent faculties and IPC experts spread across India. These experts are instrumental in bridging knowledge gaps by delivering informative lectures and workshops as part of various initiatives undertaken by CAHO. Through these educational activities, CAHO contributes significantly to enhancing the understanding and implementation of IPC measures among healthcare professionals.
By providing training and educational resources, CAHO empowers healthcare institutions to strengthen their IPC protocols and practices. This proactive approach not only helps in preventing the spread of infections within healthcare settings but also contributes to overall improvements in patient safety and quality of care.
Through innovative programs, education campaigns, and engaging stakeholders, this organisation is at the forefront of raising awareness, advocating for policy changes, and implementing evidence-based strategies to mitigate the spread of infections. By fostering partnerships with healthcare providers, government agencies like WHO India, ICMR, and local authorities like IMA, CAHO shapes a more resilient and proactive approach to infection prevention and control, ultimately contributing to improved public health outcomes across the nation.
To train healthcare professionals, CAHO launched a basic course in hospital infection control in 2018 and an advanced course in 2019, certifying a total of 4,626 participants in the basic course and 458 in the advanced course. Additionally, CAHO partners with other training academies to provide nurses with training in skill development, biomedical waste management, and disinfection strategies. In 2023, CAHO initiated a national-level online proctored certification examination – Certified Infection Control Professional (CICP). Recognising the Central Sterile Service Department (CSSD) as crucial to infection prevention and control in hospitals, CAHO-3M launched a CSSD ACE program for hospitals.
By providing training and educational resources, CAHO empowers healthcare institutions to strengthen their IPC protocols and practices. This proactive approach not only helps in preventing the spread of infections within healthcare settings but also contributes to overall improvements in patient safety and quality of care.
In addition to routine programs and trainings, CAHO recently collaborated with the World Health Organisation India on a project titled “Assessing, Brainstorming, and Documenting Issues and Challenges Faced by Healthcare Facilities with Respect to Biomedical Waste Management in the Country and Aid Compliance.” Biomedical waste (BMW) refers to any waste generated during the diagnosis, treatment, or immunisation of human beings or animals, research activities related to these, or production/testing of biological materials. Scientific disposal of BMW through segregation, collection, and environmentally sound treatment minimizes adverse impacts on health workers and the environment.
Healthcare has become one of India’s largest sectors in terms of revenue and employment, growing at a CAGR of 22% since 2016. However, it generates large quantities of waste, including sharps and infectious non-sharp wastes, requiring adequate segregation, treatment, and disposal to prevent direct and indirect health effects and environmental impact. The Biomedical Waste Management (BMWM) Rules, 2016, govern the management of biomedical waste in India.
During the COVID-19 pandemic, tens of thousands of tonnes of extra medical waste strained healthcare waste management systems worldwide, highlighting the need for improved waste management practices. India, ranked 120 among 165 nations for sustainable development, suffers from insufficient waste treatment provisions and amenities. As per the BMWM Rules, 2016, all healthcare facilities must establish mechanisms for effective BMW disposal.
Many healthcare facilities collaborate to identify effective ways to manage waste and improve compliance. It is crucial to have platforms facilitating discussions on healthcare sector problems and their management. CAHO, in collaboration with WHO India, aims to provide such opportunities. As part of this project, a training module was developed by experts in infection control, waste management, and environmental engineering, in consensus with national and state guidelines. The module included PowerPoint presentations, published guidelines, and a literature review, reviewed by WHO India experts. Addressing knowledge gaps, a 3W concept (What, Where, Why) was used in waste management teaching, clarifying material types, colour codes, and disposal reasons. Regional workshops were conducted in 2023, followed by a live simulation-based skill station workshop.
Many healthcare facilities collaborate to identify effective ways to manage waste and improve compliance. It is crucial to have platforms facilitating discussions on healthcare sector problems and their management. CAHO, in collaboration with WHO India, aims to provide such opportunities.
A gap analysis survey questionnaire, comprising eight sections and 144 questions, was circulated among workshop participants using the IBHAR app. Approximately 270 hospitals responded. Results are being analysed, and a final report is forthcoming. Two model centres, CMC Vellore and Dr Ambedkar Institute of Medical Sciences, Mohali, participated as nodal centres, conducting training of trainers and gap analysis rectification with project support.
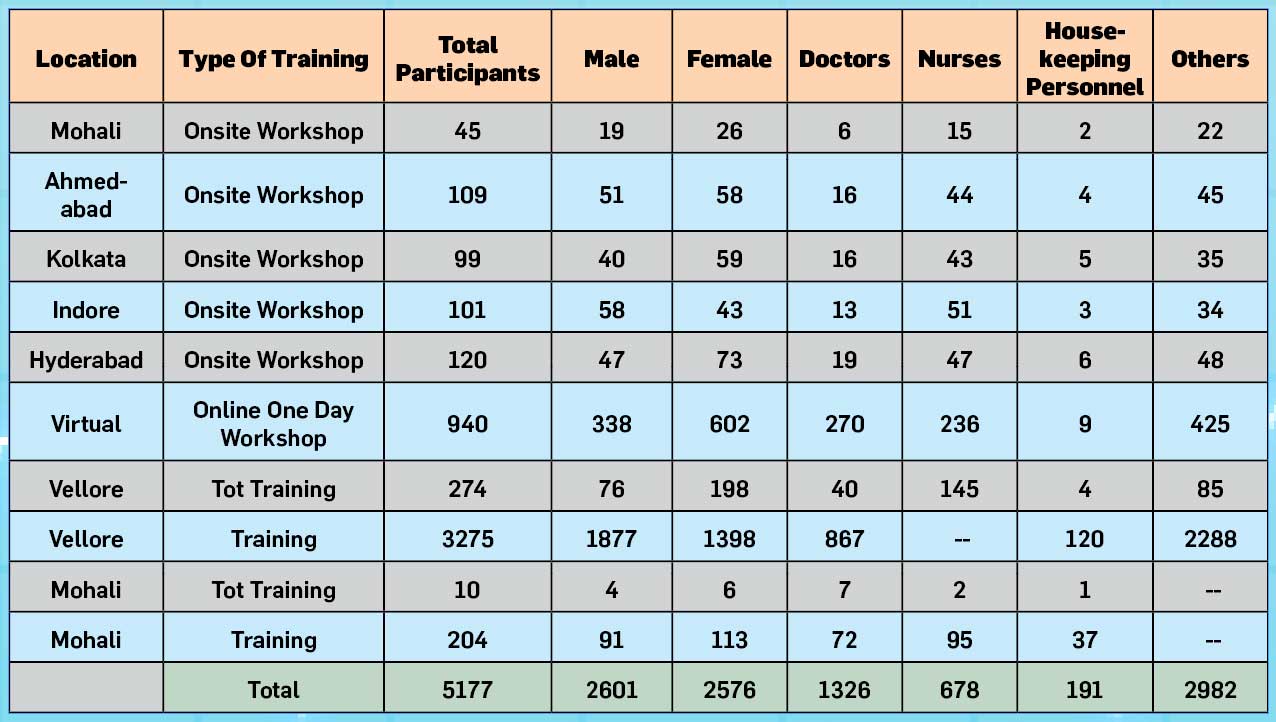
Overall Training Statistics
Lessons LEARNED from WHO BMW CAHO Project
The WHO BMW CAHO project has provided valuable insights into the challenges and shortcomings in biomedical waste (BMW) management practices within healthcare facilities. Some key lessons learned include:
Lack of Standardised Training Programs: Despite waste management being a part of medical curriculum and routine training programs, there is a common gap in knowledge and practices. This is often attributed to the absence of standardised training programs and inadequate evaluation methods during training sessions.
Need for Diverse Learning Tools: Traditional PowerPoint-based training programs may not effectively address the complexities of waste management, especially considering the wide range of medical products used in clinical practice. Utilising diverse learning tools, such as interactive discussions and hands-on activities, can enhance participants’ understanding and retention of crucial information.
Customised Training Approaches: Tailoring training sessions to the specific needs of participants and clinical settings can significantly improve comprehension and application of waste management principles. Encouraging participants to list materials used in their areas and discussing appropriate colour coding for each product is one effective approach.
Utilisation of Feedback Mechanisms: Gathering feedback from participants and addressing frequently asked questions (FAQs) can help in refining training materials and addressing common challenges faced by healthcare facilities. This iterative process ensures that training programs remain relevant and effective.
Qualitative Synthesis of Challenges: Conducting group discussions and gap analysis surveys with participants provides valuable insights into the challenges faced by healthcare facilities in waste management. This qualitative synthesis helps in identifying areas for improvement and guiding future interventions.
Takeaways
To conclude, through innovative programs, education campaigns, and community outreach efforts, not-for-profit organisations like CAHO are at the forefront of raising awareness, advocating for policy changes, and implementing evidence-based strategies to mitigate the spread of infections. By fostering partnerships with healthcare providers, government agencies, and local communities, these organisations are shaping a more resilient and proactive approach to infection prevention and control, ultimately contributing to improved public health outcomes across the nation..
(The author is Associate Consultant in the Department of Infectious Diseases and serves as the Hospital Infection Control Officer at Meenakshi Mission Hospital and Research Centre in Madurai, Tamil Nadu.)

