NUTRITIONAL MANAGEMENT of CHRONIC KIDNEY DISEASE
Whenever Chronic Kidney Disease (CKD) progresses on to dialysis, nutrition and diet play an important role in patient’s rehabilitative care. Between various dialysis treatment sessions, the wastes can build up in blood and make condition worse. A kidney friendly diet reduces waste build up in the blood and overcomes problem of malnutrition by controlling what patients eat and drink……..
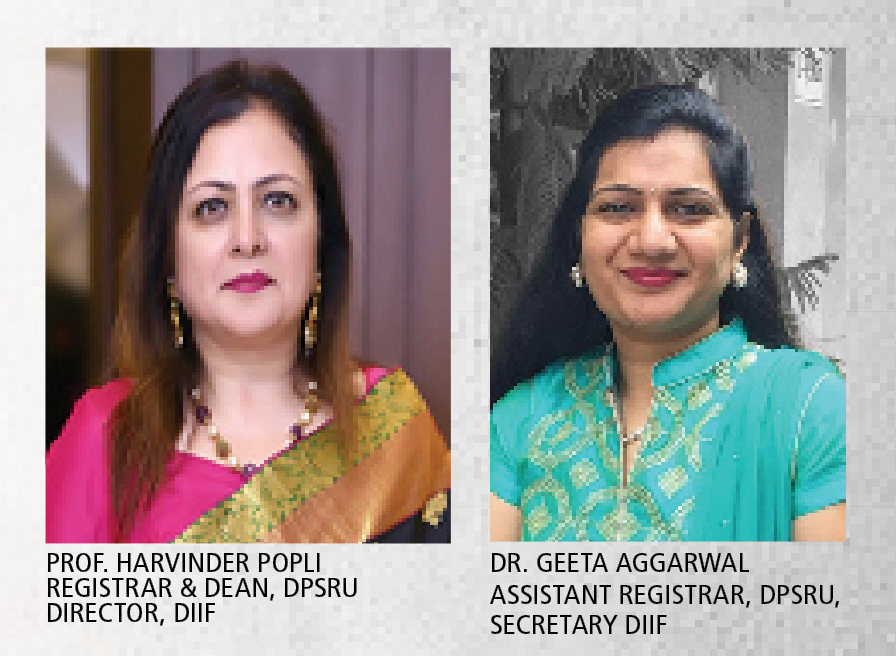
By Dr Harvinder Popli and Dr Geeta Aggarwal
Malnutrition has been seen as an important feature of chronic kidney disease (CKD). Extent of malnutrition depends on the stages of CKD. It has been observed that 50% to 70% of patients with end-stage renal disease are malnourished. Malnutrition is seen in patients on peritoneal dialysis as well as on hemodialysis. Many studies have shown that it is associated with increased mortality in the patients. Te causes of malnutrition may be the loss of appetite, impaired digestion and absorption, metabolic acidosis and emotional stress.
Dialysis helps to do some of the work that your kidneys did, when they were healthy. But dialysis cannot do everything that healthy kidneys do. Some waste and fluid may still build up in your body, especially between dialysis treatments. Over time, the extra waste and fluid in your blood can cause heart, bone and other health problems. So a well-balanced diet is necessary for them to stay fit as their kidneys are no longer functioning at its full capacity i.e. to get rid of the waste products and fluid from their blood.
It is essential for dialysis patients to have the right amount of protein, calories, fluids, vitamins & minerals each day; take medication correctly as prescribed by the doctor; comply with their dialysis treatment & do not skip any dialysis session and being physically active as possible.
Healthy diet for peritoneal or hemodialysis patients:
Getting the right amount of energy/calories
Food gives us energy. Getting the right amount of calories is important to overall health and well-being. The energy need of each individual is different and depends on age, gender, body size, physical activity level and medical condition such as kidney failure.

Need of adequate protein
Protein is essential for building and repairing muscles and daily growth. During peritoneal or hemodialysis, some amount of proteins is lost and therefore, patients require a higher protein intake compared to people who are not on dialysis. Eating the right amount of protein will help dialysis patients stay fit, as insufficient protein intake could result in weight loss, muscle wasting, reducing the ability to fight infections and thus leading to malnutrition.
Protein can be of high and low quality. For dialysis diet, high-quality protein, e.g., meat, poultry, fish and egg whites are more desirable. Most dairy products such as yogurt, milk and cheese also contain high-quality protein.
Protein food also contains phosphate. Therefore it is very important that dialysis patients take their phosphate binders with their meals.
Most people on dialysis need to limit Potassium, Phosphorus, Fluids and Sodium in their diet.
Need of less of sodium in diet
Most people should limit the amount of sodium in their diet regardless of kidney disease. Even if salt (a major source of sodium) is not adding during cooking, sodium can still be found in other food sources. This is because sodium is naturally found in all different types of foods, and more commonly in packaged and processed foods. Sodium is like-hydrated sponge that absorbs fluid. It makes you feel thirsty and intends to drink more. As a result, weight gain from fluid arises and consequently, increasing in blood pressure can be observed. Sodium restriction in kidney disease helps to maintain normal fluid balance.
Restriction in sodium intake includes: addition of limited salt during cooking; avoid using stock cubes and gravy browning e.g. Bovril, Marmite; avoid taking bottled chicken extracts; avoid taking food items that has more than 250 mg of sodium per serving; minimize the usage of canned food; use fresh herbs and whole spices in replace of salt in cooking and use fresh lime, or vinegar to flavour food.
The salt substitutes may contain high potassium, so patients should take caution about it.
Need of less of Potassium
Potassium is a mineral which is important for the nerves and muscles function. Potassium needs to be maintained at a safe level in the blood. Excessive potassium level in the blood can cause muscle weakness, abnormal heart rates and in extreme cases, heart failure.
Since hemodialysis can only remove a fixed amount of potassium, it is crucial to control the amount accumulated through patient dietary intake. Potassium is found mainly in fruits and vegetables, with small quantities found in nuts, dry beans and dairy and meat products.
It is important to avoid high potassium food like wholegrain cereals, bread and biscuit; nuts, seeds and related products, e.g. chocolate, peanut butter; coconut milk, kaya; fresh/canned fruit and vegetable juice, herbal medicine drinks, strong tea/coffee, cocoa and malted beverage, milk, wine; brown sugar, molasses, maple syrup, toffees, liquorice; high potassium salt substitute, bottled sauces, meat and vegetables extract, essence of chicken, stock cube and fruits and vegetables from the high potassium group.
 Potassium can be reduced in the vegetables by leaching and socking.
Potassium can be reduced in the vegetables by leaching and socking.
Need of less of phosphorus
As the kidneys become less effective at filtering waste products, blood phosphate level rises. When it begins to build up in the blood, calcium is drawn from the bone. The calcium phosphate product forms hard deposits in patient’s tissues leading to skin itchiness, joint pain, and eye irritation and hardens their blood vessels. Over time, patients’ bones become weak and brittle. This leads to fractures and constant pain.
Both hemodialysis and peritoneal dialysis patients need to control the amount of phosphate in their diet. Almost all patients with high phosphate levels will also need to take phosphate binders as most foods contain some amount of phosphate. Usually phosphate binders are taken within 5 to 10 minutes before or immediately after meals and snacks. Phosphate binders prevent the body from absorbing the phosphate from the foods eaten and thus helping to prevent renal bone disease.
Phosphorus binders work in one of two ways. Some phosphate binders, such as Renvela (Calcium and Aluminium free phosphate binder), work like a sponge and soak up the phosphates in the food so that it doesn’t get into the blood. Instead it is carried through the digestive tract and eliminated in the stool. Other phosphorus binders, such as Fosrenol (Calcium and Aluminium free phosphate binder), Phoslo and Tums (Calcium based phosphate binders), work like a magnet. The phosphorus in the food connects to the phosphorus binder and it is carried through the digestive tract to be eliminated.
Calcium-based phosphorus binders have largely replaced aluminum-based binders and may also serve as calcium supplements. Calcium acetate, also called PhosLo, is one commonly used phosphorus binder. There are many others, usually containing calcium carbonate. Tums is a form of calcium carbonate, which can also be effective. Because most people need to take several phosphate binders with every meal, there may be concern about dialysis patients absorbing too much calcium from these medicines, so calcium levels must be monitored. Aluminum-free, calcium-free phosphorus binders, such as Renagel (sevelamer) and Renvela (sevelamer carbonate), mix with phosphorus in the intestinal tract, but do not contain aluminum or calcium, so they don’t cause problems with excess aluminum or calcium load. Chewable Fosrenol (lanthanum carbonate) is another aluminum and calcium free binder. Aluminum-based phosphorus binders and Magnesium based phosphorus binders are used rarely, when other binders are not effective.
 Food rich in phosphorus that patients need to avoid when they have high serum phosphate levels include: oats, cereals; dairy products; bone-based soups; bean products (all forms of nuts, seeds, bean soup); chocolate and related products; malt drinks (e.g. Milo, Horlicks, Ovaltine); processed food and canned food (e.g. canned meat or fish, sausage, meat patty); organ meats (e.g. liver, intestine); seafood, sardines, anchovies (ikan bilis) and dried shrimp paste and wholegrain and related products (e.g. wholemeal bread, brown rice, wholemeal noodles)
Food rich in phosphorus that patients need to avoid when they have high serum phosphate levels include: oats, cereals; dairy products; bone-based soups; bean products (all forms of nuts, seeds, bean soup); chocolate and related products; malt drinks (e.g. Milo, Horlicks, Ovaltine); processed food and canned food (e.g. canned meat or fish, sausage, meat patty); organ meats (e.g. liver, intestine); seafood, sardines, anchovies (ikan bilis) and dried shrimp paste and wholegrain and related products (e.g. wholemeal bread, brown rice, wholemeal noodles)
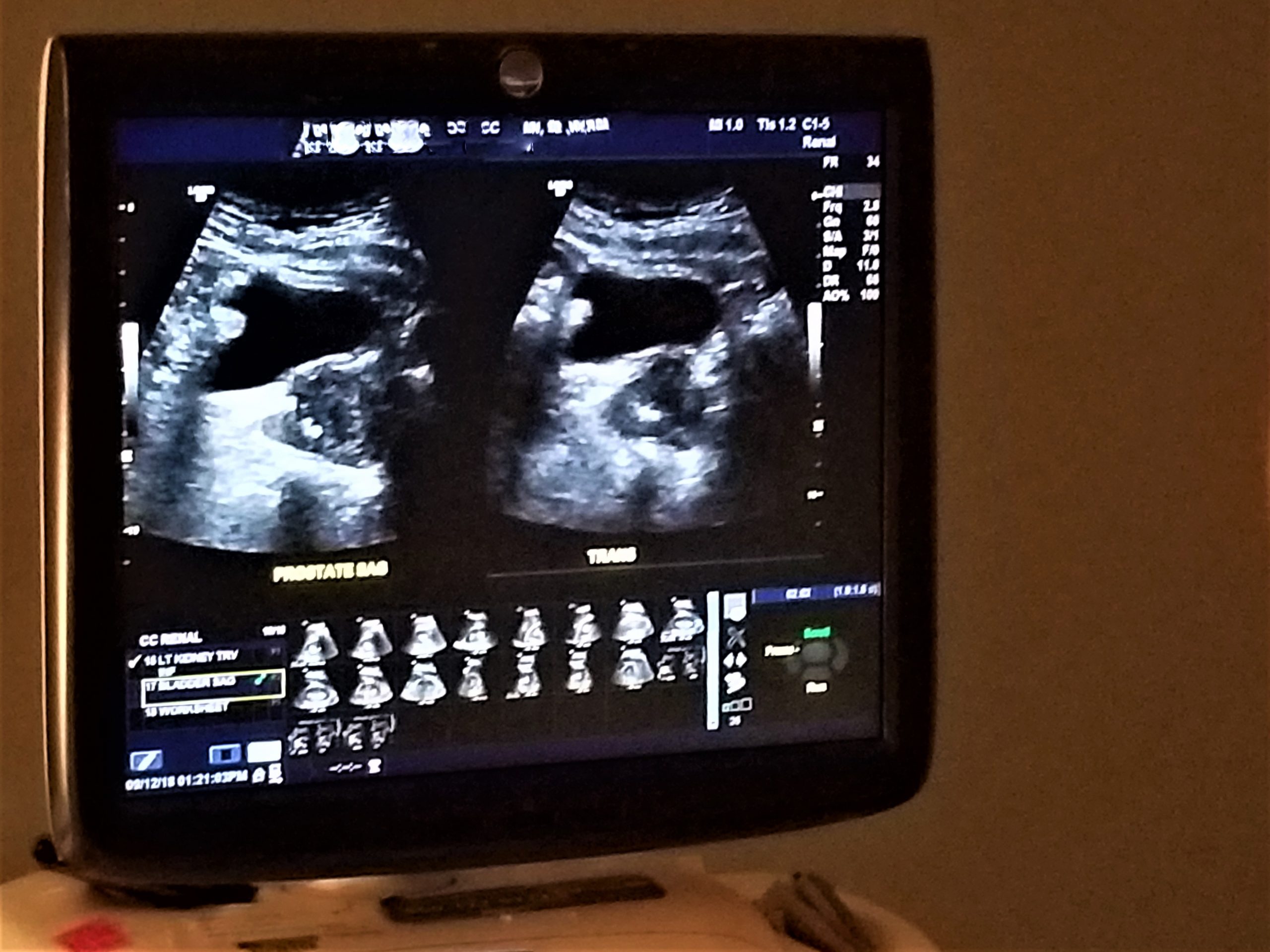
Need of control in intake of fluids
Dialysis removes extra fluid from your body. However, it can remove only limited fluid at a time safely. If you come to your hemodialysis with too much fluid in your body, your treatment may make you feel ill. You may get muscle cramps or have a sudden drop in blood pressure that causes you to feel dizzy or sick to your stomach. Excess fluid can build up in your body and may cause swelling & weight gain between dialysis sessions; changes in your blood pressure; the heart to work harder, which can lead to serious heart trouble and a buildup of fluid in your lungs, making it hard for you to breathe.
One way to limit how much liquid you have is to limit the salt in the foods you eat. Salt makes you thirsty, so you drink more. Foods that are liquid at room temperature, such as soup, contain water. Gelatin, pudding, ice cream, and other foods that include a lot of liquid in the recipe also count. Most fruits and vegetables contain water, such as melons, grapes, apples, oranges, tomatoes, lettuce, and celery. When you count up how much liquid you have in a day, be sure to count these foods.
Prevention of anemia
Anemia is common among dialysis patients and it appears to be more common in those who suffer from malnutrition or protein energy wasting. Symptoms of anemia include fatigue, weakness, dizziness, headache, low immunity, breathless or shortness of breath, chest pain, low appetite and pale.
Anemia of CKD is one of the complications of kidney failure. Its severity can be related to how well the kidney is functioning. The main reason for anemia among chronic disease patients is the reduced production of erythropoietin (EPO) by the kidneys. EPO prompts the bone marrow to make red blood cells. When the kidney’s function is decreasing, the amount of EPO produced will be reduced. Other factors that cause anemia among dialysis patients are: reduced red blood cell lifespan due to accumulated urea toxic; lack of iron; lack of folate and other vitamins and blood loss during hemodialysis.
Adequate intake of protein, iron, vitamin B 12 and folate are important in preventing and treating anemia as these nutrients are the important elements in making new red blood cells.
Vitamins and Minerals in Kidney Disease
Vitamins and minerals are substances, which body needs to help carry out special functions. They provide energy, help the body to grow and repair tissue and maintain life. But if a patient is on dialysis, he/she may not get enough nutrients.
Almost all vitamins and minerals come from the foods we eat. The body cannot make these substances. People with healthy kidneys who eat a variety of foods from all the food groups (meats, grains, fruits, vegetables and dairy products) can get lots of vitamins and minerals. But if they have kidney disease or are on dialysis, the diet may limit some food groups; therefore, body may not get all the vitamins and minerals that is needed each day. Some vitamins are lost during dialysis treatment. There is need to take some in the form of supplements.
Depending on the health and other factors, the healthcare provider may recommend some of the following supplements:
B Complex: B complex vitamins are grouped together, but each has a different job to do.
One of the important functions of vitamin B6, B12 and folic acid is to work together with iron to prevent anemia. If patient has anemia, it means he/she has not enough red blood cells. Red blood cells carry oxygen from the lungs to all parts of your body. Additional B vitamins, called thiamine, riboflavin, pantothenic acid and niacin, can also be given as a supplement.
Iron: If the patient is taking medicine to treat anemia, he/she may also need to take an iron pill or have injectable iron. It should be taken only if healthcare provider prescribes it.
Vitamin C: Vitamin C is used to keep many different types of tissue healthy. It also helps wounds and bruises heal faster and may help prevent infections. The healthcare provider may need to give a prescription for these vitamins.
Vitamin D: The patient may also need to take some vitamin D. It can be given as a pill and can also be given during dialysis treatment. In addition to maintaining healthy bones, newer research shows that vitamin D may also protect against heart disease. There are different types of vitamin D. Vitamin D sould be taken, if healthcare provider prescribes it.
Calcium: Calcium along with vitamin D helps to keep bones healthy. It is important to take only the amount of calcium prescribed by doctor or dietitian. Too much calcium can clump together with phosphorus and deposit in places such as your heart, blood vessels, lungs and other body tissues. If blood phosphorus level is too high, there is need to take a medicine used to bind the phosphorus from your food. Some phosphorus binder medications contain calcium. They can give extra calcium if needed.
Vitamins that are needed to avoid in CKDThere is need to avoid some vitamins and minerals during kidney disease. Some of these include A, E and K. These vitamins are more likely to build up in the body and can cause harm. Over time, they can cause dizziness, nausea, and even death. These vitamins can be taken with the prescription of doctor. There is also some concern about vitamin C. Although some people may need to take a low dose of vitamin C, large doses may cause a buildup of oxalate in people with kidney disease. Oxalate may stay in the bones and soft tissue, which can cause pain and other issues over time.
•Herbal Supplements and Kidney Disease
We may think about using herbal supplements to help with any health concerns, but in case of a patient with kidney disease, one should use caution with herbal supplements.
Use of herbal supplements is often unsafe if one has kidney disease since some herbal products can cause harm to the kidneys and even make the kidney disease worse. Also, your kidneys cannot clear waste products that can build up in your body.
Herbal supplements that are especially risky for patients with any stage of kidney disease, who are on dialysis or who have a kidney transplant include Astragalus, Barberry, Licorice Root, Parsley Root, Apium Graveolens, Horsetail, Oregon Grape Root, Cat’s Claw etc.
Some herbal supplements that act like a diuretic or “water pill” may cause “kidney irritation” or damage. These include Bucha leaves and Juniper berries. Uva ursi and parsley capsules may also have bad side effects. Many herbal supplements can interact with prescription drugs. A few examples are St. Johns Wort, echinacea, ginkgo, garlic, ginseng, ginger and blue cohosh. If one has a kidney transplant, they are especially at risk, as any interaction between herbal supplements and medicines could put them at risk for losing your kidney.
Points to remember:
•Important to know:
If patient does peritoneal dialysis, he/she may be able to take in slightly more phosphorus, potassium, sodium and fluid, than if he/she did hemodialysis. One also needs to eat more protein. This is because peritoneal dialysis works all day and night to take waste and fluid out of your blood. This keeps the waste and fluid from building up in your blood like it does between hemodialysis treatments. So the diet plan can be different in both cases of dialysis.
•Special diet for patients with diabetes
If patient is diabetic, the diet plan will be different that allows him/her to avoid the nutrients that are needed to limit, while also controlling the blood sugar. If patient does peritoneal dialysis, keep in mind that peritoneal dialysis solution has dextrose in it. Dextrose is a type of sugar. When the dialysis is done, some of the dextrose is taken in by the body. So it is very important to count the dextrose in dialytic solution as extra sugar in the diet. Conversation with doctor and dietician is important in this case.
•Conclusion:
Proper nutrition is essential to reduce morbidity and mortality in CKD patients. Nutrition is often neglected in CKD patients while more focus is placed on modalities of dialysis and on transplant. A proper diet history, nutritional assessment and counseling are an important cornerstone of CKD therapy.
Increased use of medications that are prescribed at any given point of time to a patient with CKD or patient on dialysis creates havoc on his gastrointestinal system. Phosphorus binders may result in constipation while other medications may cause diarrhoea, heartburn, stomach-ache, vomiting and kill the good bacteria in the gut. Thus, probiotics may seem promising in helping restore the good bacteria in the gut and thereby improving immune function and providing anti –inflammatory effects if taken with the consultation with healthcare provider.
Many nutritional supplements are available in the market. These may be in the form of powders, which are low in potassium and phosphate. These can provide 7-10 kcal/kg calories and 0.3-0.4 g/kg protein. Patients on dialysis may be given as intradialytic parenteral nutrition. Patients on peritoneal dialysis may benefit from amino acid based dialysis solutions.
Some patients tend to over-eat unhealthy foods while at other extreme others restrict almost all food stuffs. CKD diet does not mean a restricted diet. In fact most patients even with CKD can adopt a healthy diet with minor modifications especially those highlighted above.
(The authors are from Delhi Pharmaceutical Sciences & Research University, New Delhi)

